Embarking on the journey of transition can be a very exciting time for a transgender individual. Finally being able to match their outward appearance to their gender identity can do wonders for their mental health and confidence.
Hormone therapy is a common first step in the transition process, but there is very little education on how hormone therapy can affect the urinary tract.
However, there are things that can be done to manage the changes that will come with hormone therapy and other transitional processes.
*It should be noted that although this blog specifically uses transgender language, this information also applies to non-binary individuals who are also seeking hormone therapy.
Does Estrogen Cause Urinary Incontinence?
Transgender women are individuals who were designated male at birth.
When beginning hormone therapy, transgender women often take high levels of estradiol medications as well as anti-androgens (spironolactone and finasteride are the typical beginning medications). These medications target the lower urinary reproductive system by blocking testosterone production.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
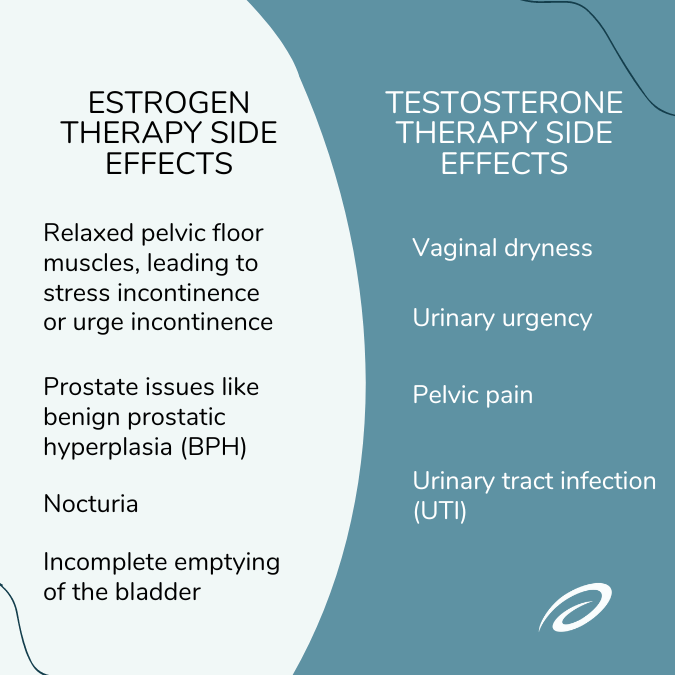
Hormone Side Effects
- Relaxed pelvic floor muscles, leading to urinary incontinence, such as stress incontinence or urge incontinence.
- Prostate issues, such as benign prostatic hyperplasia (BPH).
- Nocturia
- Incomplete emptying of the bladder.
Helpful Treatments
- Pelvic floor physical therapy (PFPT): A pelvic floor physical therapist can be enormously helpful for transgender patients going through hormone therapy. A licensed pelvic floor physical therapist can work with you to resolve or ease some of your symptoms.
- Removal of the testes & estrogen therapy: One of the leading side effects associated with estradiol and anti-androgen medications is issues with the prostate. Removal of the testes in addition to estrogen therapy can decrease the risk for BPH, also known as an enlarged prostate. This form of treatment can also help minimize the potential for urinary tract symptoms that often accompany BPH, including urinary frequency or urgency, nocturia, and incomplete emptying of the bladder. It should also be noted that prostate cancer is more common among transgender women that begin hormone therapy over the age of 50.
Does Testosterone Therapy Cause Urinary Incontinence?
Transgender men, or individuals who were assigned female at birth, often begin the transition process by taking high levels of testosterone.
Testosterone medications act to block ovarian function, which in turn decreases estrogen levels. While this is an effective method to change outward appearance, there are side effects that individuals should be aware of before they begin to take hormone supplements.
Hormone Side Effects
- Vaginal dryness.
- Urinary urgency.
- Pelvic pain.
- Urinary tract infections (UTIs).
While these side effects may not be eliminated completely, there are ways to help minimize them and make the individual more comfortable.
Helpful Tips
- Avoid products that are highly fragranced. Personal products like bubble baths, highly perfumed soaps, lubricants, etc. can exacerbate vaginal dryness and irritation and should be avoided, if possible.
- Consider natural lubricant alternatives. A few natural lubricant options are coconut oil, aloe vera, and vitamin E.
- Stay hydrated. Staying hydrated raises your body’s overall moisture levels. This is key to easing vaginal dryness and decreasing your chances of frequent UTIs.
- Try probiotics. Some individuals have found that probiotics help alleviate vaginal dryness. However, it is important to talk with your healthcare provider about the best way to introduce probiotics into your routine.
If you begin to experience pelvic pain or dysfunctional voiding, it may be helpful to seek help from a pelvic floor physical therapist. Dysfunctional voiding occurs when there is inconsistent coordination between the bladder and the urethra. Signs of voiding dysfunction include frequent urination, urinary urgency, and the inability to completely empty the bladder. Whether you are experiencing symptoms or not, regularly seeing a pelvic floor therapist can be very beneficial in resolving issues ranging from painful intercourse to incontinence issues.
What Is the Best Way to Prevent Urinary Incontinence?
-
Pelvic floor therapy. You can begin seeing a pelvic floor physical therapist before starting hormone therapy to ensure that your pelvic floor is strong. You can also make an appointment with a therapist after starting hormone therapy to solve any issues you may be experiencing.
-
Eat the right foods. Certain foods can irritate your bladder which can increase symptoms of urinary incontinence. Avoid foods the following foods to prevent urinary incontinence:
-
Spicy foods.
-
Tomato-based foods.
-
Carbonated drinks.
-
Alcohol and caffeine.
- Foods with synthetic dyes.
-
- Exercise regularly. Exercise is good for your overall physical health and urinary health. You can also incorporate pelvic floor exercises into your routine, like kegels. These can be done by both men and women!
- Use incontinence products. If you’ve been diagnosed with urinary incontinence, you may qualify to get bladder care supplies for free through your insurance plan. Adult protective underwear and bladder control pads are excellent options for those experiencing lighter urinary leakage. These discreet products will catch leaks and stop odors, keeping you feeling fresh while you navigate your incontinence treatment plan.
Gender Confirmation Surgery
For some transgender individuals, the next step to affirming their gender identity is undergoing gender affirmation surgery.
There are multiple surgeries available to individuals who elect to surgically transition their gender. As with any surgical procedure, there are risks, and it is important to consult with your healthcare provider on any questions you have about potential complications. It should also be noted that not all transgender people choose to, or can afford to, undergo medical procedures that will be listed below, and this is perfectly fine.
Healthcare Resources for Transgender Individuals
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.