Key Takeaways:
-
Roughly 32 million adult Americans experience incontinence, and about 1 in 7 men has urinary incontinence.
-
If you have Medicaid or insurance, you may qualify for free incontinence supplies like male guards, adult briefs, or diapers through Aeroflow Urology.
-
Male incontinence can stem from an enlarged prostate, prostate cancer treatment, nerve damage, an overactive bladder, pelvic floor muscle changes, diet-related bladder irritants, or certain medications.
Male urinary incontinence (UI) is a common condition that affects millions of men worldwide. It can lead to social isolation, financial strain, and mental health issues. However, you’re not alone. Men of all ages can manage incontinence, and with the right treatment and products, you can take back control.
With so many men managing in silence, it’s time to start having transparent conversations. This article explores the causes of male incontinence, treatment options, and how you can receive products like adult briefs or male guards.
What Is the Main Cause of Incontinence in Men?
There are a variety of reasons that men may be experiencing symptoms of urinary incontinence. Most cases are tied to prostate changes, often benign prostatic hyperplasia (BPH), also known as an enlarged prostate.
When the prostate enlarges, it can slow or block urine flow, leading to a weak stream, frequent trips to the bathroom, and incomplete emptying.
Other causes for male bladder issues include:
-
Aging: As we age, our pelvic floor muscles may become weak and atrophy without regular strength and resistance training. This can result in diminished ability for the urinary sphincter to efficiently adapt to changes in pressure, leading to leakage.
-
Constipation: Chronic constipation can create hard stool, which can press on the bladder. Excessive straining to defecate overworks the pelvic muscles and reduces continence.
-
Waist circumference: Increased abdominal girth and waist circumference raise pressure on the bladder and pelvic floor, contributing to stress incontinence in men.
-
Diet: Certain foods and beverages can irritate the bladder lining, which can lead to symptoms of urge incontinence. Common culprits include citrus, spicy foods, caffeine, alcohol, and even dehydration.
-
Neurological conditions: Nerve changes can disrupt bladder signaling. Some of the most common conditions include diabetes, Parkinson’s disease, multiple sclerosis, spinal cord injuries (SCIs), Alzheimer’s disease, herniated discs, and stroke.
-
Urinary tract infections (UTIs): Less common in men than in women, UTIs are infections that occur when bacteria enter the urethra and infect the urinary tract.
-
Smoking: A chronic cough from smoking can repeatedly stress the pelvic floor and lead to urine leakage.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Types of Male Urinary Incontinence
There are two primary types of urinary incontinence in men: urge incontinence and stress incontinence. A urologist can confirm your diagnosis and design your treatment plan around the type of urinary incontinence you are experiencing.
1. Urge Incontinence
Sometimes called overactive bladder, urge incontinence is the more common type of UI in men. This type of urinary incontinence is the involuntary loss of urine following a sudden and strong urge to urinate.
Urge incontinence can happen when pelvic nerve damage occurs from pelvic or abdominal surgeries. It can also occur after spinal cord injuries (including herniated discs), and is often seen in neurologic conditions such as Parkinson’s disease, multiple sclerosis, and diabetes, which can damage the nerves supplying the bladder.
2. Stress Incontinence
Less common than urge incontinence, stress urinary incontinence occurs when leakage happens when coughing, laughing, sneezing, lifting, or jumping. The pressure from these activities overcomes the muscles holding the bladder and urethra shut.
It is less common in men than in women, but it can occur after a prostatectomy (partial or full removal of the prostate gland) or from chronic coughing due to long-term smoking.
Other types of incontinence include overflow incontinence (dribbling when you pee), functional incontinence, and mixed incontinence. Mixed incontinence occurs when an individual has more than one type of UI.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Treatments for Male Incontinence
While urinary incontinence treatment varies from person to person, it can usually be treated. Always talk with a clinician about a plan that fits your unique needs before starting any lifestyle changes:
Pelvic Floor Retraining
Work with a pelvic floor physical therapist or occupational therapist. They can assess pelvic floor tone and muscle coordination across the pelvis, abdominals, and lower back to address what’s causing leaks.
Several pelvic floor exercises, such as Kegel exercises or pelvic floor muscle stretches, can also be worked into your exercise routine to help strengthen the pelvic floor. Despite what the stigma says, pelvic floor exercises aren’t just for women — men can do them, too!
Eating For Your Bladder
Avoid foods and drinks that irritate your bladder, such as citrus, spicy foods, caffeine, excessive alcohol, and sugar. Staying hydrated can also help prevent constipation, which in turn supports your bladder function.
Using Male Incontinence Products
Incontinence products, such as male bladder control pads and male protective underwear (also called adult briefs), are discreet ways to control leaks. They can be worn at work, at home, while exercising, and while enjoying other activities throughout your day.
Submit your information, call your doctor, select your free products, and we'll ship them to you each month in discreet packaging.
Urinating When Needed
Voiding (emptying your bladder) every 2 to 3 hours is important to avoid overfilling, urgency, and potential leaks.
Bladder Training
Taking the time to train your bladder can also be a helpful way to treat your incontinence. Review your plan with a healthcare provider to match your symptoms and goals.
Why Don’t Men Talk About Incontinence?
Many men don’t discuss UI symptoms with their loved ones or even their healthcare providers.
A study by the National Association for Continence (NAFC) reported that 27% of people experiencing UI don’t talk about it with their doctor despite needing help managing symptoms. Another study concluded that only 1 in 5 men with weekly leakage had ever sought treatment.
What Stigmas Surround Male Incontinence?
About 32 million Americans live with incontinence, yet stigma still follows, labeling male UI as “shameful,” "embarrassing," or “gross.”
This could be because we often treat natural bodily functions — like passing gas or urine leaks — as taboo topics, which may prevent people from seeking help.
The truth is that emptying our bladders is a normal part of life. Bladder control issues also don’t discriminate; men, women, children, teenagers, adults, and seniors can develop urinary incontinence for many reasons.


What Effect Does Incontinence Have on Men?
As a result of stigmas, incontinence can make life difficult, both physically and emotionally. Nearly 90% of people with UI report feeling isolated or hopeless.
Urinary incontinence in men can even lead to:
- Concerns about masculinity.
- Fear of losing bodily control.
- Work disruption (or missing work).
- Anxiety or depression.
- Feeling self-conscious about frequent bathroom trips.
Studies also show that men with urinary conditions such as nocturia (waking up during the night to pee) are at higher risk for developing depression.
Five Ways to Support Men with Urinary Incontinence
Male incontinence is real, but the stigma doesn’t have to remain. Whether you or someone you love experiences incontinence, know that there are practical ways to break the silence and move toward treatment:
- Stay active. Leaks don’t have to sideline you. Use men's incontinence products to confidently keep exercising, seeing friends, or doing what you enjoy.
- Talk about it. Openness reduces stigma. If you’re close to someone who has UI, let them know you’re there for support. Or, if you have urinary incontinence, try to bring it up with your clinician to explore your options.
- Continue learning. Educate yourself on the different types of urinary incontinence and fecal incontinence.
- Seek support from loved ones. Speak to your loved ones about what you’re going through. Find someone who is non-judgmental and make sure it’s someone you’re comfortable around.
- Find community. Knowing that you aren’t alone in managing UI can provide a sense of relief. Join a moderated group, online or in person, to compare tips on products, routines, and treatments. Anonymous forums and patient groups can also point you to practical resources and questions to ask at your next doctor’s appointment.
If you have Medicaid or insurance, you may qualify for free incontinence supplies like adult briefs through Aeroflow Urology. Call us at 1-844-276-5588 (Monday - Friday: 8:00 AM - 6:00 PM ET) or email info@aeroflowurology.com.


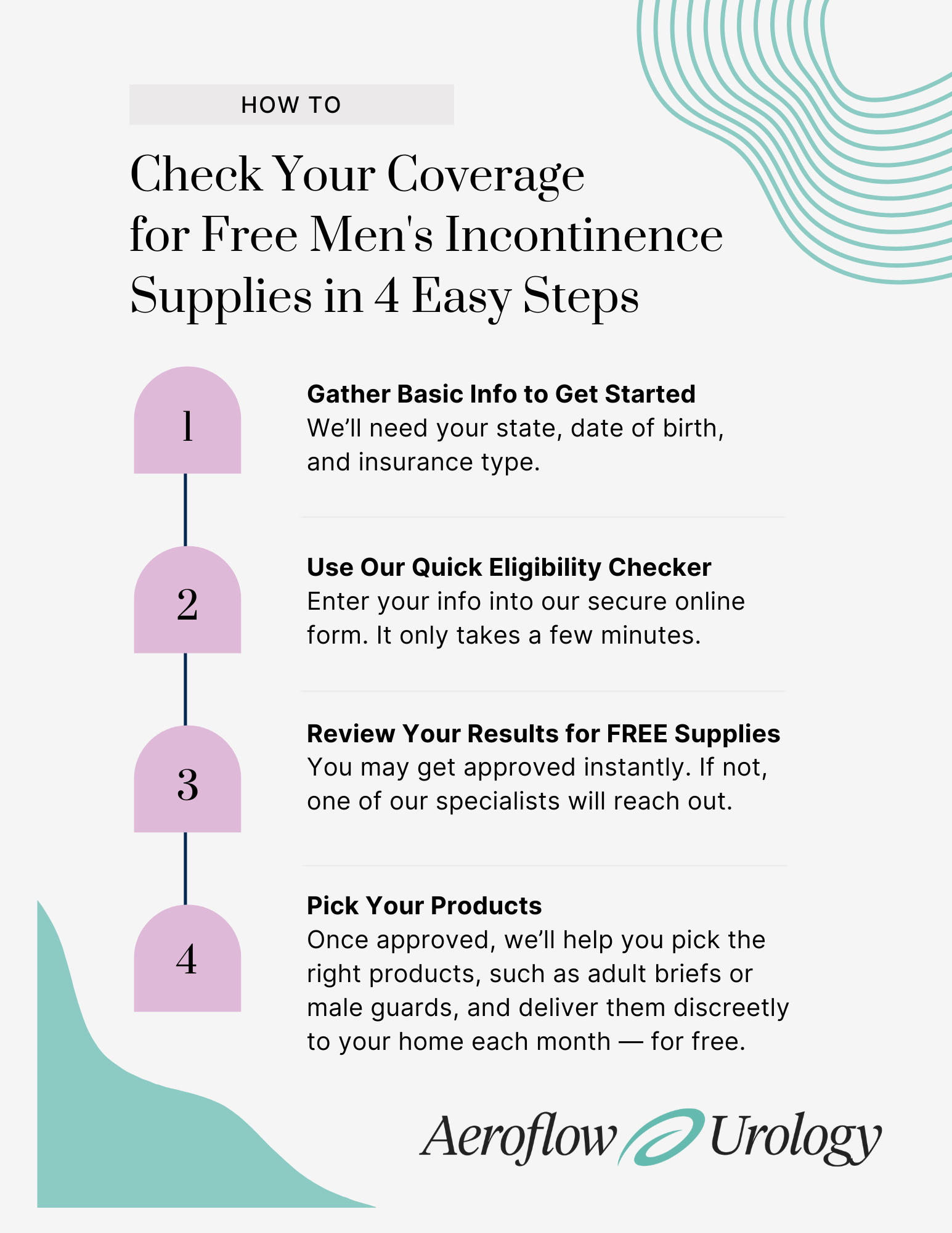
Check Your Eligibility for Free Men’s Bladder Care Products
Nearly 1 in 7 men in the U.S. experiences bladder leaks, but most don’t talk about it. If that’s you or someone you love, know that help is available.
At Aeroflow Urology, we work with your insurance and healthcare provider to confirm eligibility for free incontinence supplies. If you qualify, we’ll ship your $0 monthly products, like adult briefs or male guards, directly to your door in discreet packaging. Reordering your no-cost supplies is also easy with one-click emails and one-word “Yes” replies to our reorder texts.
Start saving up to $630 each month on men’s bladder control supplies today.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Frequently Asked Questions
What are the best male incontinence products?
The best male incontinence products depend on how much you’re leaking (light to heavy incontinence), and the type of incontinence (urinary, fecal, or mixed) you have. Common options include male guards, protective underwear (pull-ups), and adult briefs (also called adult diapers). Booster pads and underpads (chux) can add extra protection.
Are male incontinence supplies covered by insurance?
Yes, Medicaid or insurance can cover the cost of incontinence supplies. If you qualify through Aeroflow Urology, you may be able to get your male bladder control supplies for free each month, delivered to your home in discreet packaging. You can also easily reorder with one-click texts or by email.
What’s the difference between stress and urge incontinence in men?
Stress incontinence typically happens during movement, like coughing, sneezing, or lifting heavy objects, often due to weak pelvic muscles or post-surgery changes. Urge incontinence (overactive bladder) feels like a sudden, strong need to urinate, and can be linked to nerve conditions, bladder irritants like caffeine or alcohol, or certain medications.
What are the most common causes of male bladder issues?
Male bladder problems are often caused by benign prostatic hyperplasia (enlarged prostate), weak pelvic floor muscles, or an overactive bladder. Nerve conditions like Parkinson’s or a past stroke can affect bladder control. Other causes include urinary tract infections, constipation, and bladder irritation from drinking caffeine or alcohol.
Why do I dribble when I pee?
You may be experiencing overflow incontinence, which happens when your bladder is too full. A clinician can confirm the cause and suggest the right treatment options.
Is there urinary incontinence medication for men?
Yes, medication is available, but it’s usually considered after pelvic floor therapy and lifestyle changes. The proper medication depends on the cause, such as an overactive bladder or prostate issues. An overactive bladder may respond to anticholinergics or beta-3 agonists, while prostate issues may need alpha-blockers or 5-alpha reductase inhibitors.
References
Breyer, B. N., Kenfield, S. A., Blaschko, S. D., & Erickson, B. A. (2014). The association of lower urinary tract symptoms, depression and suicidal ideation: data from the 2005-2006 and 2007-2008 National Health and Nutrition Examination Survey. The Journal of urology, 191(5), 1333–1339. https://doi.org/10.1016/j.juro.2013.12.012
Harris, S. S., Link, C. L., Tennstedt, S. L., Kusek, J. W., & McKinlay, J. B. (2007). Care Seeking and Treatment for Urinary Incontinence in a Diverse Population. Journal of Urology, 177(2), 680–684. https://doi.org/10.1016/j.juro.2006.09.045
Harvard Health Publishing. (n.d.). Better bladder and bowel control: Practical strategies for managing incontinence. Harvard Health. Retrieved November 6, 2025, from https://www.health.harvard.edu/digestive-health/better-bladder-and-bowel-control-practical-strategies-for-managing-incontinence
Irwin, D. E., Kopp, Z. S., Agatep, B., Milsom, I., & Abrams, P. (2011). Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU international, 108(7), 1132–1138. https://doi.org/10.1111/j.1464-410X.2010.09993.x
Jenkins, S. (2019, November 5). Overcoming the stigma of incontinence. National Association for Continence. https://nafc.org/bhealth-blog/overcoming-the-stigma-of-incontinence/
Markland, A. D., Richter, H. E., Fwu, C. W., Eggers, P., & Kusek, J. W. (2011). Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. The Journal of urology, 186(2), 589–593. https://doi.org/10.1016/j.juro.2011.03.114
Nitti, V. W. (2001). The prevalence of urinary incontinence. Reviews in Urology, 3 (Suppl 1), S2–S6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1476070/
Shamliyan, T. A., Wyman, J. F., Ping, R., Wilt, T. J., & Kane, R. L. (2009). Male urinary incontinence: Prevalence, risk factors, and preventive interventions. Reviews in Urology, 11(3), 145–165. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777062/
Stothers, L., Thom, D., & Calhoun, E. (2005). Urologic diseases in America project: Urinary incontinence in males—Demographics and economic burden. The Journal of Urology, 173(4), 1302–1308. https://doi.org/10.1097/01.ju.0000155503.12545.4e
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.