Key Takeaways:
- Urinary incontinence can be a side effect of prostate surgery, but there are many ways to manage it, including pelvic floor exercises, medications, and bladder training.
- You may be eligible for free bladder control products like pads and catheters through your insurance, helping to relieve the pressure of incontinence post-prostate cancer surgery.
- After prostate surgery, there may be different types and stages of male incontinence treatment options depending on the severity of leakage.
Jump To:
How Does Prostatectomy Cause Urinary Incontinence?
What Are the Different Stages of Urinary Incontinence After Prostatectomy?
What Are the Signs of Urinary Incontinence After Prostate Surgery?
7 Tips for Managing Urinary Incontinence After Prostatectomy
How to Keep Your Prostate Healthy
Can I Get Free Bladder Control Products After Prostate Surgery?
There are moments in life that redefine us. For many men, the battle against prostate cancer is one such moment. It's a journey marked by strength, hope, and the unwavering determination to regain control of your life.
Yet, an intimate struggle is often faced silently, hidden beneath a veil of stigma: urinary incontinence. For those who have undergone a prostatectomy, this challenge can be a daunting and emotionally turbulent part of recovery. It's not just a physical hurdle but an emotional one, testing the limits of one's self-esteem and sense of normalcy.
This article will discuss urinary incontinence after a prostatectomy, providing the best tips for managing urinary leakage and other conditions that may develop after prostate cancer surgery. Use this post to regain control over your body and restore the confidence and dignity that cancer may have momentarily taken away.
What Is Urinary Incontinence?
Urinary incontinence (UI), or the loss of bladder control, is a medical condition where one loses control of their bladder, typically leading to symptoms like urine leakage, dribbling, and frequent urination.
UI is common in men; about 1 in 4 experience urinary incontinence, and about 1 to 8.4% experience urinary dysfunction after prostate surgery.
How Does Prostatectomy Cause Urinary Incontinence?
With typical bladder function, urine remains in your bladder until you empty it. When you void the bladder, urine leaves your body through the urethra, forcing your bladder muscles to contract. Your internal urethral sphincter muscles relax as the bladder muscles contract and allow urine to flow.
During a prostatectomy, you may have the valve that dictates urine flow and your prostate removed. With these removals, you may experience muscle or nerve damage as a side effect. Your prostate gland surrounds your urethra, so it can be challenging for your body to control urine flow following prostate surgery.
You may also experience UI after prostate cancer treatments, such as radiation therapy.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
What Are the Different Stages of Urinary Incontinence After Prostatectomy?
Several types of UI you may experience after a prostatectomy fall into the categories of urinary control, voiding, and leakage issues. Your symptoms may range from less intense incontinence to severe incontinence.
While most men recover from prostate surgery after about 4 to 6 weeks, UI symptoms can last longer. Some men manage symptoms for a short period, while others may have symptoms that last for weeks, months, or years.
Stress urinary incontinence and post-void dribbling are the most common types of male incontinence. UI can occur after prostate cancer treatments like radiation therapy. Some men may also experience erectile dysfunction (ED) following surgery.
Other common types of UI and other conditions that may develop following prostate surgery include:
- Post-Void Dribbling: Dribbling urine after emptying your bladder.
- Urge Incontinence / Overactive Bladder (OAB): Feeling a strong and intense impulse to urinate that occurs suddenly, sometimes resulting in urine dribble.
- Stress Incontinence: Leaking urine when sneezing, laughing, lifting heavy objects, or exercising.
- Mixed Incontinence: Experiencing two or more sets of UI symptoms at once.
- ED: Inability to maintain an erection during sexual intercourse.
Speak with your healthcare provider or urologist to determine which type of UI you're experiencing.
What Are the Signs of Urinary Incontinence After Prostate Surgery?
Common signs that you may have UI include:
- Leaking urine when coughing, sneezing, exercising, running, lifting heavy objects, or bending over.
- Dribbling urine after emptying your bladder.
- Feeling the intense and sudden urge to urinate, leading to leakage.
- Feeling the urge to void your bladder more frequently than usual.
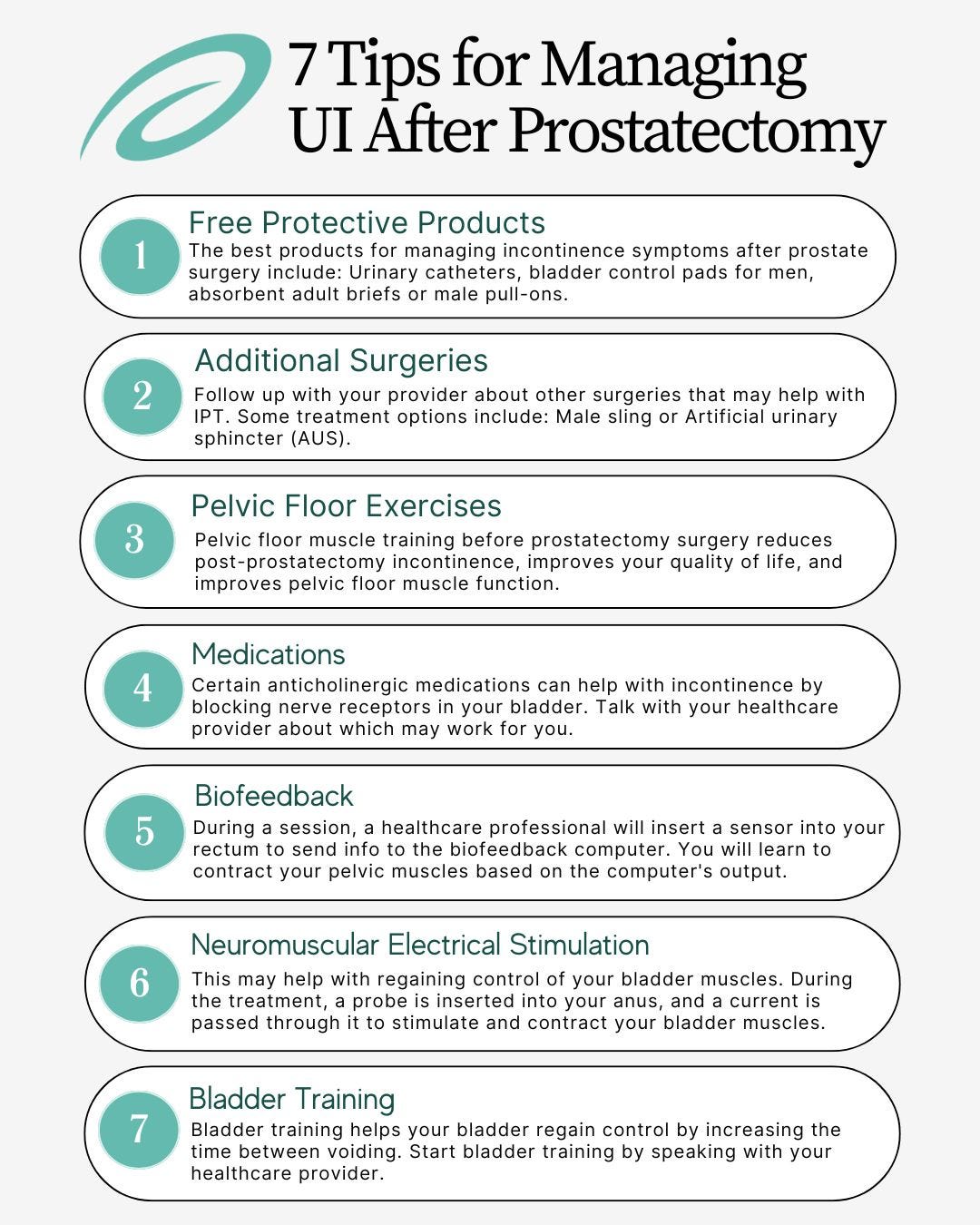
7 Tips for Managing Urinary Incontinence After Prostatectomy
1. Free Protective Products
Use bladder control products to manage your UI symptoms following surgery. These supplies can help ease the stress of urine leaks and keep you comfortable all day. You may be able to get these products through Aeroflow Urology if you have Medicaid or another private insurance plan, so check if you qualify with our secure Eligibility Form!
The best products for managing incontinence symptoms after prostate surgery include:
If you do qualify to receive products through Aeroflow Urology, we'll send you free samples, connect you with a Continence Care Expert, and ship your products on a monthly basis directly to your door in discrete, unmarked boxes for free!
2. Additional Surgeries
Follow up with your provider about other surgeries that may help with IPT. Some treatment options include:
- Male sling: This is a minimally invasive treatment wherein a mesh-like tape is placed around the urethral bulb. This moves the urethra into a different position and helps with incontinence.
- Artificial urinary sphincter (AUS): AUS can help you if you have a weak sphincter muscle. First, an inflatable cuff is placed around your upper urethra and closes to prevent leakage. Next, a pump in the scrotum helps open and close the cuff. A small pressure-regulating balloon is also placed under the abdomen that holds urine back.
3. Pelvic Floor Exercises
Pelvic floor muscle training before prostatectomy surgery reduces post-prostatectomy incontinence, improves your quality of life, and improves pelvic floor muscle function. Engaging your pelvic floor muscles after surgery strengthens them and improves bladder control. Kegel exercises can also speed up your recovery time. You can also see a pelvic floor therapist for extra guidance.
4. Medications
Certain anticholinergic medications can help with incontinence by blocking nerve receptors in your bladder. Talk with your healthcare provider about which may work for you. These include:
- Enablex
- Vesicare
- Ditropan XL.
- Detrol LA.
- Oxytrol patch.
- Oxybutynin 3% gel.
- Imipramine
5. Biofeedback
Weekly biofeedback sessions can lessen UI symptoms. During a session, a healthcare professional will insert a sensor into your rectum to send information to the biofeedback computer. Then, you will learn to contract your pelvic muscles based on the computer's output.
6. Neuromuscular Electrical Stimulation
Neuromuscular electrical stimulation may help with regaining control of your bladder muscles. During the treatment, a probe is inserted into your anus, and a current is passed through it to stimulate and contract your bladder muscles.
7. Bladder Training
Bladder training helps your bladder regain control by increasing the time between voiding. Start bladder training by speaking with your healthcare provider. They may recommend holding your urine for around 5 minutes when you feel the urge to go and increasing that hold time by 5 minutes. Continue until you're able to hold your urine for an average period.
How to Keep Your Prostate Healthy
Follow these guidelines to stack the deck in your favor of keeping your prostate healthy.
1. Engage In Regular Physical Activity
Engage in regular physical activity that includes both aerobic and resistance training. The Physical Activity Guidelines for Americans recommends:
- Aerobic: 30 minutes a day for a minimum of 150 minutes per week of the aerobic challenge is needed (70-80% HR max).
- Strength: 2 to 3 times weekly for all the major muscle groups.
2. Go Plant-Based
A more plant-focused diet improves overall health and can lower your risk of prostate cancer.
3. Ejaculate More or Less?
One research study suggests that men who reported a high ejaculation frequency (reported as ≥ 21 ejaculations per month) may have a lower risk of prostate cancer. It is important to note that those who reported low ejaculation frequency (0-3 times per month) also had decreased risk for prostate cancer. This data is inconclusive and not predictive of ejaculation frequency associated with the level of prostate cancer risk. Many other variables may be associated with this lower risk (lifestyle factors, age, family history of prostate cancer, prostate screening, etc.).
4. Reduce Stress
Reduce physiological burden and consequences of unrelenting, unmanaged stress (proinflammatory cellular response, oxidative stress). You can do this by practicing mindfulness techniques, such as meditating, journaling, or exercising.
5. Get More Sleep
Preliminary research shows that poor sleep may be associated with an increased risk of prostate cancer, so aim to get the recommended amount of sleep for your age range.
6. Get Prostate Screenings at the Right Time
Although this is controversial, screenings may help prevent or detect early prostate cancer. The American Urological Association's guidelines state:
- PSA screening is not recommended for men under 40 years old.
- Routine screening is not recommended in men between the ages of 40 to 54 years old.
- The most significant benefit of screening appears to be in men ages 55 to 69 years old at average risk.
- PSA screening in men 70+ years old or any man with less than a 10 to 15-year life expectancy is not recommended.
- A screen may benefit those 70+ if they are in excellent health.
Can I Get Free Bladder Control Products After Prostate Surgery?
Managing incontinence can be overwhelming at times. However, Aeroflow Urology can assist in supplying incontinence supplies through your Medicaid (and some private insurance) plan. This service is financially beneficial and alleviates stressful store trips, especially if you're facing some bathroom challenges!
How It Works: Instead of running out to the store for bladder control supplies at the last minute, you can get them delivered to your doorstep in discreet packaging on a monthly basis... for FREE if you qualify!
To see if you can receive our services, fill out our Eligibility Form today. It's quick and easy to do. Then, if approved, one of our Continence Care Experts will reach out to your healthcare provider for a required prescription on your behalf. After receiving your prescription, we'll contact you within 1 to 2 business days with the next steps. You'll be able to ask for free product samples before confirming your shipment and refill your supplies every month with the help of our friendly text or email reminders.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.
References:
UpToDate. (n.d.). www.uptodate.com. Retrieved March 15, 2022, from https://www.uptodate.com/contents/urinary-incontinence-after-prostate-treatment#:~:text=Incontinence%20after%20simple%20open%20prostatectomy
Nam, R. K., Herschorn, S., Loblaw, D. A., Liu, Y., Klotz, L. H., Carr, L. K., Kodama, R. T., Stanimirovic, A., Venkateswaran, V., Saskin, R., Law, C. H. L., Urbach, D. R., & Narod, S. A. (2012). Population Based Study of Long-Term Rates of Surgery for Urinary Incontinence After Radical Prostatectomy for Prostate Cancer. Journal of Urology, 188(2), 502–506. https://doi.org/10.1016/j.juro.2012.04.005
Park, J. J., Kwon, A., Park, J. Y., Shim, S. R., & Kim, J. H. (2022). Efficacy of pelvic floor exercise for post-prostatectomy incontinence: Systematic review and meta-analysis. Urology. https://doi.org/10.1016/j.urology.2022.04.023
Milios, J. E., Ackland, T. R., & Green, D. J. (2019). Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urology, 19(1). https://doi.org/10.1186/s12894-019-0546-5
Eastham, J. A., Kattan, M. W., Rogers, E., Goad, J. R., Ohori, M., Boone, T. B., & Scardino, P. T. (1996). Risk Factors for Urinary Incontinence after Radical Prostatectomy. Journal of Urology, 156(5), 1707–1713. https://doi.org/10.1016/s0022-5347(01)65488-0
Koch, M. O., Nayee, A. H., Sloan, J., Gardner, T., Wahle, G. R., Bihrle, R., & Foster, R. S. (2003). Early catheter removal after radical retropubic prostatectomy: long-term followup. The Journal of Urology, 169(6), 2170–2172. https://doi.org/10.1097/01.ju.0000065860.16392.19
OUP accepted manuscript. (2021). The American Journal of Clinical Nutrition. https://doi.org/10.1093/ajcn/nqab365
Leitzmann, M. F. (2004). Ejaculation Frequency and Subsequent Risk of Prostate Cancer. JAMA, 291(13), 1578. https://doi.org/10.1001/jama.291.13.1578