Key Takeaways:
-
Meltdowns are not intentional outbursts but medical events triggered by overwhelm, sensory overload, or anxiety.
-
Watch for early signs of meltdowns, like increased stimming, fatigue, sensory distress, or regression. Being aware of these signs helps caregivers respond with calm and safety-focused support.
-
Understanding sensory needs, maintaining structure, fostering autonomy, and learning effective coping mechanisms through professional guidance are key to preventing and managing meltdowns.
Jump To:
Recognizing the Warning Signs: 6 Things to Look Out For
How to Help: Before & During a Meltdown
Long-Term Strategies for Lessening Meltdowns
What Does an Autistic Meltdown Look Like?
How Can I Support Someone During an Autistic Meltdown?
How to Get Free Incontinence Supplies Through Insurance
Have you ever witnessed someone seemingly lose complete control, overwhelmed by intense emotions? If your loved one is autistic, it could be an autistic meltdown.
These experiences are often misunderstood and mistaken for a temper tantrum, but the two are quite different.
Let's delve deeper into what meltdowns truly are and how we can better understand and offer appropriate support to loved ones who experience them.
What Are Autistic Meltdowns?
An autistic meltdown is an involuntary occurrence, a temporary loss of emotional regulation where an individual appears to have lost complete control over their emotional state. It's not a deliberate act; rather, it's a medical event or occurrence tied to a medical condition or diagnosis. These events are often driven by stressors like sensory overwhelm or overload, changes in routine, or difficulties with transitions. Feelings of anxiety can also play a significant role.
When a neurodivergent person faces an intensely stimulating environment – think too much noise, overpowering smells, or large crowds – it can become overwhelmingly overstimulating, triggering a "fight or flight" response. Meltdowns can manifest in various ways, including emotional outbursts, loss of speech, and a diminished ability to cope with everyday sensory and social demands. Many describe it as an "explosion of emotion.”
It's crucial to remember that meltdowns vary widely in intensity, duration, and behavioral characteristics. Some common traits include:
- Crying
- Yelling and screaming.
- Hitting or slapping.
- Biting or kicking.
- Throwing objects.
- Rocking
- Growling
- Head banging or other self-injurious behaviors.
- Flopping down.
As an observer, the intense emotions driving these behaviors might seem to appear suddenly, for no obvious or apparent clear reason, and can escalate quickly.
Meltdowns Are Never Anyone's Fault
It's paramount to understand that meltdowns are nobody's fault. They are not intentional attempts to control a situation or another person. Instead, they are involuntary stress responses characterized by raw emotion and feelings of overwhelm, overload, or being beyond functioning capacity.
Unfortunately, meltdowns are sometimes misinterpreted as typical temper tantrums. This highlights the critical need for accurate knowledge, public education, and advocacy. If someone you know is experiencing intense emotional responses that seem like meltdowns, especially if they are undiagnosed, it’s a strong indicator that medical assessment and/or treatment is necessary.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Recognizing the Warning Signs: 6 Signs to Look Out For
Being aware of potential triggers and pre-meltdown signs can be incredibly helpful. Here are some things to watch for:
- Increase in stimming: This could involve loud verbal stimming or rapid repetitive movements like hand flapping or rocking.
- Signs of temporary regression: This might include a loss of speech in someone who is usually verbal or the sudden inability to perform skills they typically have.
- Complaints of tiredness without napping: This can indicate a need to be alone to decompress and self-regulate, sensing they are overwhelmed.
- Visible signs of sensory overload: This can include putting hands over ears, excessive fidgeting, humming, or making unusual sounds as a way to self-regulate.
- Changes in character: An individual might become unexpectedly sad, quiet, or withdrawn.
- Changes in temperament: They might become loud, angry, irritated, snap at others, or display bigger emotions than usual.
If intense rage or aggression is present, it's crucial to monitor the situation calmly. Avoid touching the person, as this could add another common trigger or provoke fear, and keep others away. Advocate for them and seek support from a mental health professional if needed. In unsafe situations, don't hesitate to call for emergency assistance. Safety is always the top priority!
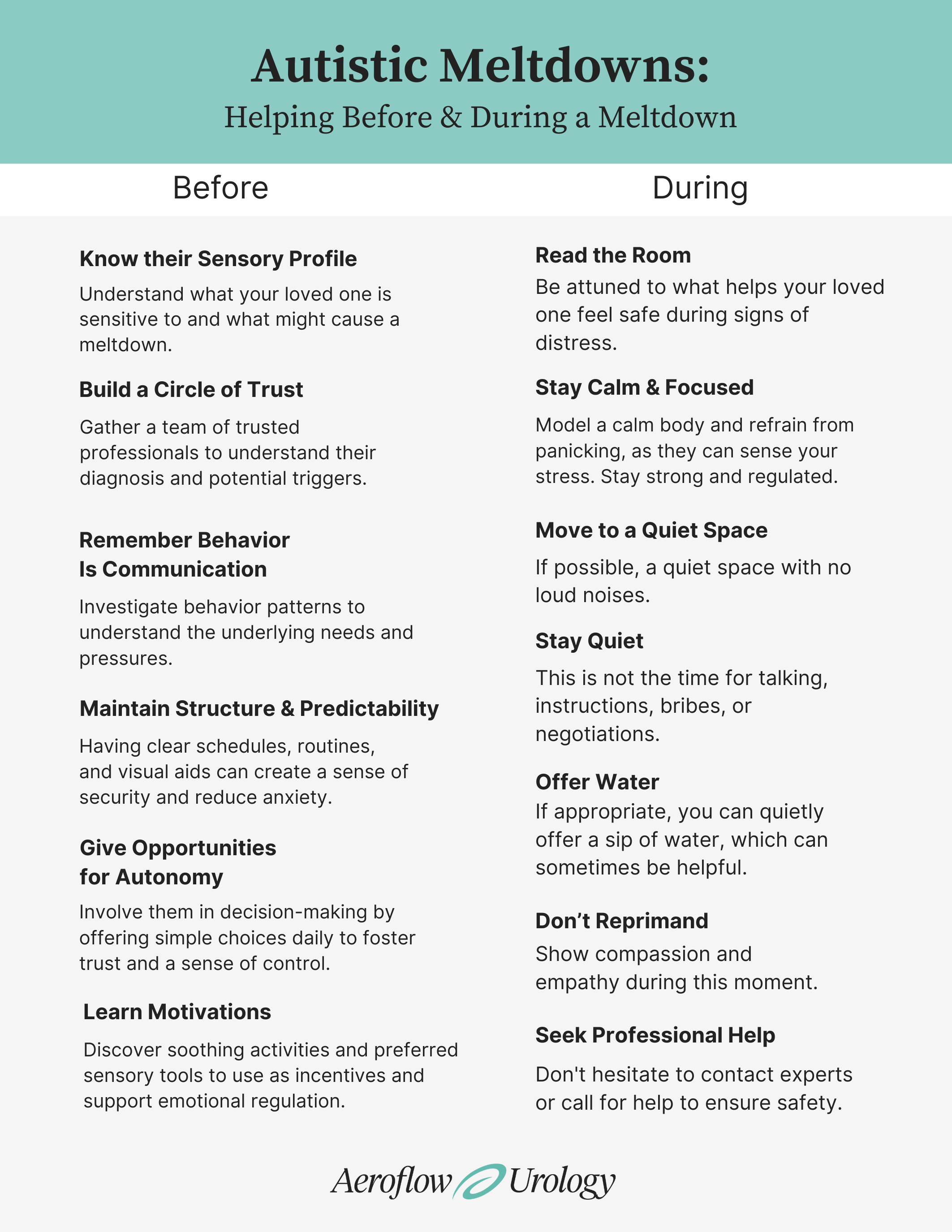
How to Help: Before & During a Meltdown
Beforehand (Preventing Meltdowns):
- Know your loved one's sensory profile: Understand their sensitivities and tolerances. They might be hypersensitive to some sensory stimuli and hyposensitive to others. Seeking an assessment from an experienced occupational therapist or a sensory support integration therapist is highly recommended.
- Build a "circle of trust": Gather a team of trusted professionals to understand their diagnosis and potential triggers. Consider a referral to an experienced psychiatrist for dangerous behaviors or mental health concerns.
- Remember all behavior is communication: Investigate behavior patterns to understand the underlying needs and pressures. Help them develop self-regulation and coping mechanisms. Effective communication is a fundamental human right; consider a referral to a speech-language pathologist if needed for speech, language, or communication aids.
- Maintain clear structure and predictability: Having clear schedules, routines, and visual aids can create a sense of security and reduce anxiety.
- Offer opportunities for autonomy: Involve them in decision-making by offering simple choices daily to foster trust and a sense of control.
- Learn what motivates them: Discover soothing activities and preferred sensory tools to use as incentives and support emotional regulation. Consider creating a sensory corner or room at home.
During a Meltdown:
- Read the room: Be attuned to what helps your loved one feel safe during signs of distress.
- Stay calm and focused: Model a calm body and refrain from panicking, as they can sense your stress. Stay strong and regulated.
- Consider moving them somewhere with no loud noises: If possible, a quiet space like a car or a room with noise-cancelling headphones might help.
- Be quiet! This is not the time for talking, instructions, bribes, or negotiations.
- Quietly offer a sip of water if appropriate: Sometimes this can be helpful.
- Never reprimand or undermine them: Show compassion and empathy during this moment of crisis.
- Seek professional help if necessary: Don't hesitate to contact experts or call for urgent help to ensure safety.
Being proactive is key to thinking clearly, acting quickly, and maintaining a good trusting relationship in the long term.
Long-Term Strategies for Lessening Meltdowns
- Work on sensory solutions: Begin with a sensory integration assessment or occupational therapy. Maximize opportunities for sensory input like alone time, sensory tools, and breaks throughout the day. Ensure these are included in their IEP at school. Speech therapy can also help with communication.
- Maintain clear structure and predictability: As mentioned before, this helps reduce anxiety.
- Offer opportunities for autonomy: Include them in decision-making to build trust and reduce anxiety.
- Learn what motivates them: Incorporate preferred sensory tools and activities into their environment.
Meltdown vs. Temper Tantrum: Understanding the Key Differences
Distinguishing between a meltdown and a temper tantrum is crucial for appropriate responses.
Meltdown
- Before: Often triggered by overwhelm, sensory overload, or challenges with transition and change.
- During: Involuntary loss of control, may be unaware of surroundings.
- After: Needs time to recover, may be exhausted or unaware of what happened.
- Intentionality: Not intentional, a medical event.
Temper Tantrum
- Before: Often a response to not getting a desired object or activity.
- During: Calculated behavior, often with an audience in mind.
- After: Often stops immediately once the desired outcome is achieved.
- Intentionality: Often intentional and manipulative.
It's also important to note that meltdowns and tantrums can sometimes occur together in sequence, especially in individuals with intellectual disabilities or developmental delays.
What Does an Autistic Meltdown Look Like?
The image of a loud, outwardly explosive meltdown isn't always accurate. Meltdowns can also be more silent, where an individual might stim excessively, hum, or whine quietly. This still indicates intense emotions and a need to escape the environment. Look for signs like:
- Suddenly and quietly fleeing a situation.
- Signs of a stress or fear response (rapid heartbeat, shaking, sweating).
- Total loss of speech or communication (situational mutism).
- Changes in movement, like suddenly flopping down.
- Zoning out or appearing detached.
- An increase in seemingly typical stimming like quiet humming or whining.
- Loss of ability to function in regular routines.
- Complaints of tiredness without actual rest.
The Pain & Exhaustion of Meltdowns
Be mindful of the risk of exhaustion and increased mental health concerns for individuals who experience meltdowns, as well as for the caregivers. The invisible struggles, judgment from others, and misunderstandings can be incredibly painful for everyone involved, potentially leading to caregiver burnout. Don't hesitate to reach out for medical and peer support.
Other Similar Related Conditions
- After-school restraint collapse syndrome: This refers to the emotional dysregulation some individuals experience after a demanding day of "masking" and trying to fit in. It's common in many children, not just those with disabilities, as they process a lot throughout the day. Your home is often their safe place to release these pent-up emotions.
- Autistic shutdown: Similar to meltdowns, shutdowns are also medical events where the individual becomes overwhelmed. However, instead of an outward explosion, they retreat partially or totally from their regular lives, needing complete quiet in their safe spaces. Shutdowns can last for extended periods and may be mistaken for depression. A meltdown can sometimes lead to a shutdown. When in doubt, seek professional help.
How Can I Support Someone During an Autistic Meltdown?
The world can be overwhelming for neurodivergent individuals. The persistent confusion between tantrums and meltdowns contributes to stigma, shame, and daily difficulties.
Remember, you are not obligated to over-explain personal matters to those who don't need to know. Focus on the care and safety of your loved one and advocate for accurate language to ensure their experiences are validated.
Caregiver Points for Consideration & Empowerment
As a caregiver, your well-being is crucial. Remember to:
- Seek help for your own emotional and physical well-being.
- Make a plan with professionals about what you can manage.
- Learn from the experts about triggers and prevention strategies.
- Consider behavior management and crisis response courses.
- Seek assistance from a psychiatrist for your loved one and therapy for yourself if needed.
- Explore co-regulation and emotional regulation strategies for both of you.
- Keep an open mind about potential solutions and seek respite support.
- Don't discount your own needs for support and time alone.
It's your responsibility to reduce the trauma, stigma, and incorrect perceptions surrounding disabilities. Meet your loved one where they are, learn their triggers and needs, and respond appropriately to keep them safe. Never talk negatively about them in their presence or treat their meltdowns as controllable flaws. Understand that behaviors, including meltdowns, are often a form of communication.
Important Note for Caregivers
Be mindful about oversharing details of meltdowns with people you don't trust. Never video your child during a meltdown and share it publicly. Seek support privately through trusted professionals and support groups. Protecting your loved one's dignity and privacy is paramount.
Understanding autistic meltdowns is a journey of empathy and learning. By recognizing them for what they truly are – involuntary responses to overwhelm – we can move towards providing better support, reducing stigma, and fostering a more inclusive society.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.