Our body functions as one large connected system that works together to perform basic tasks, such as emptying the bladder. However, when someone suffers a spinal cord injury (SCI), the system may no longer function properly, leading to urinary incontinence.
But patients and loved ones don’t have to fight their symptoms on their own. There are a variety of care tips to simplify caring for incontinence and SCI.
In this post, we’ll explain the ins and outs of SCI and how it affects the bladder, and we’ll also give you tips on bladder management to improve your quality of life.
IN THIS ARTICLE:
What Level of Spinal Cord Injury Causes Urinary Incontinence?
How Does Spinal Cord Injury Affect Bladder Control?
What Are the Treatments for Spinal Cord Injury & Urinary Incontinence?
How to Care for Someone With Spinal Cord Injury & Urinary Incontinence
How to Get Incontinence Products Through Insurance for Spinal Cord Injury
What Level of Spinal Cord Injury Causes Urinary Incontinence?
It’s been reported that around 80% of people who have experienced a spinal cord injury (SCI) experience a loss of bladder control, a condition known as neurogenic bladder.
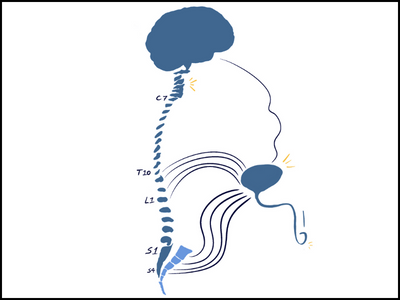
Let’s talk about basic anatomy to understand how the spinal cord and brain impact normal bladder function.
Check Your Eligibility
2 Easy Steps
From catheters to pediatric and adult incontinence supplies, discover the continence care essentials covered by your insurance.
How the Bladder Functions
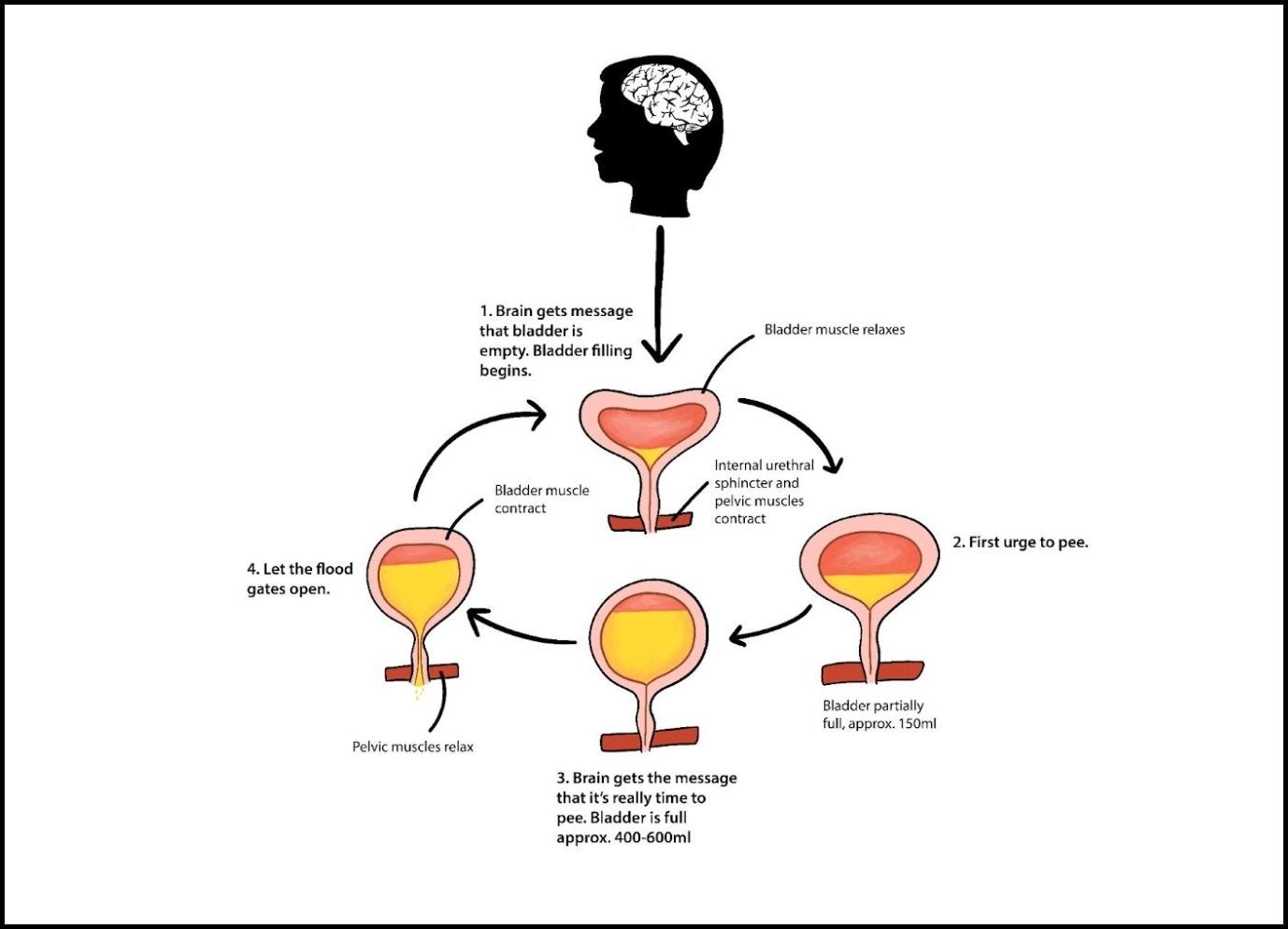
Signals to and from the spinal cord travel up and down a neural superhighway to your brain. The brain also sends signals to your spinal cord using this same pathway. The different spinal cord levels that make up your neural pathway control different bladder functions. Your bladder reflexes are similar to the reflexes in your knee. Here’s how they function.
- Your bladder fills with urine.
- The bladder’s sensory nerves (sacral spinal nerves: S1, S2, S3, S4 ) send signals to the spinal cord.
- The spinal cord responds, sending signals to the bladder to contract.
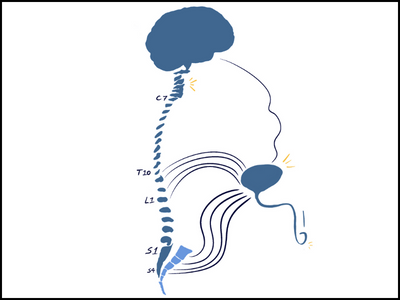
Spinal Cord Levels
T10 - L2: These spinal cord levels and their accompanying peripheral nerves are involved in:
- Bladder muscle relaxation.
- Urinary sphincter contraction.
- Storage of urine.
S1 - S4: These spinal cord levels and their accompanying peripheral nerves are responsible for:
- Sensation
- Voluntary motor control (muscle activation).
- Voluntary motor control of pelvic floor muscles, such as the urinary sphincter relaxation, bladder muscle contraction, and elimination of urine.
Bladder function depends on the level of the SCI and whether it’s complete or incomplete. To keep it simple, we’ll focus on complete SCI presentations, which occur when the nerves below the injury no longer communicate with the brain.
How Does Spinal Cord Injury Affect Bladder Control?
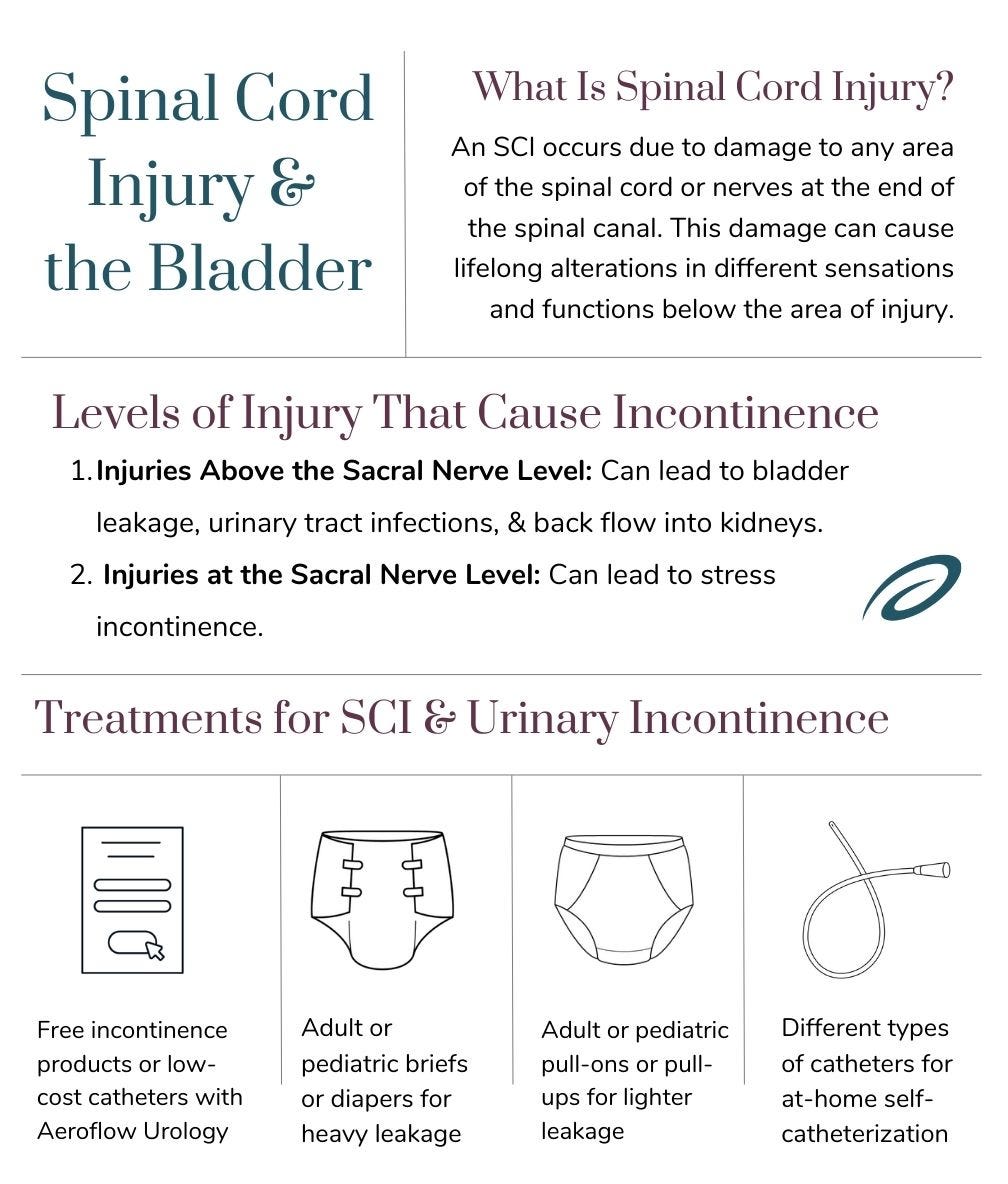
An SCI occurs when you experience damage to any area of your spinal cord or the nerves at the end of your spinal canal. This damage can cause lifelong alterations in different sensations and functions below the area of injury. Let’s look at what happens to your bladder control with each level of injury. Usually, the higher up the damage occurs, the more severe the injury is.
- Injuries above vertebrae TH12/L1: May lead to detrusor sphincter dyssynergia, or the inability to empty the bladder or control bladder impulses.
- Injuries below TH12/L1: Causes lost muscle tone of the bladder and sphincter. The ability to fully empty the bladder, hold urine, or prevent leaks may be impaired.
- Lower spinal cord injuries: May cause the inability to fully empty the bladder.
1. Injuries Above the Sacral Nerve Level
With these types of injuries, the bladder reflex does come back, but because the brain cannot communicate with the bladder and do its part, the bladder reflex takes over and runs the show. This can lead to:
- Involuntary loss of urine.
- Difficulty storing urine.
Over time, the bladder muscle contractions or spasms might intensify because your brain can’t send signals to stop the bladder’s reflex. This makes it hard for your bladder to fill up because it’s contracting faster and more often, preventing it from stretching. When this happens, the bladder walls thicken, making the bladder work harder than it needs to, causing the muscles to become stiff.
When the bladder muscle gets too stiff, it’s no longer easy for the bladder to hold urine and empty it efficiently, resulting in a high-pressure situation in the bladder. Your body always looks for the path of least resistance, which means that you’ll likely experience bladder leakage, or the urine will back up into the kidneys to accommodate this bladder pressure issue.
If the sphincter muscles are spastic, it’s difficult for urine to leave your bladder when the bladder muscle contracts. It also makes fully emptying your bladder challenging. Typically, the bladder muscle and urinary sphincter muscles around the bladder coordinate to help with the bladder filling and emptying. Still, with an SCI, these muscles work out of sync. This can lead to frequent urinary tract infections (UTIs), kidney hydronephrosis (urine backflow to the kidneys), and urinary incontinence.
2. Injuries at the Sacral Nerve Level
When these injuries occur, your bladder function is impacted slightly differently, where the bladder muscle becomes flaccid or weak. The bladder reflex is impacted and results in diminished:
- Bladder sensation.
- Urges to urinate.
- Ability to contract.
This leads to a bladder that can hold a lot of urine without you being aware of how full your bladder actually is. When you’re ready to void your bladder, it can be challenging for bladder contractions to occur.
This may result in bladder problems, such as urinary retention and forceful pushing using your abdominals to help squeeze your pee out.
Over time, your bladder, prostate, rectum, uterus, and pelvic ligaments become strained and stressed. Sometimes, pelvic organ prolapses can occur if there’s too much strain on the organs. People with SCIs at the level of the sacral spinal nerves commonly experience stress urinary incontinence, which involves leaking when coughing, laughing, sneezing, or other exertional activities.
What Are the Treatments for Spinal Cord Injury & Urinary Incontinence?
Every person’s incontinence situation is unique and should be supported individually to determine the best treatment approach for you. Here are some ways you can manage your bladder leaks. Be sure to speak to your healthcare provider before deciding which strategy is best for you.
- Catheters. Depending on your level of SCI and the type of bladder condition you have, your provider may recommend using catheters. Intermittent catheters, indwelling catheters, suprapubic catheters, or external catheters are all great options for management. Intermittent catheterization can assist in easy bladder emptying in the comfort of your home. See if you qualify for low-cost intermittent catheters through your insurance plan with Aeroflow Urology. Speak to your healthcare professional before choosing the catheter you want to use.
- Adult or pediatric briefs. Briefs (diapers) are excellent for bladder control because they are absorbent and open easily with tabs on the sides. This allows you to change your brief easily if you use a wheelchair or have less mobility. Briefs are best for those with heavier leakage.
- Adult or pediatric pull-ons. Designed to look and feel like real underwear for both males and females, pull-ons (pull-ups) are absorbent and discreet. You should use protective underwear if you have moderate leakage.
How to Care for Someone With Spinal Cord Injury & Urinary Incontinence
If a loved one or patient has spinal cord injury symptoms that include incontinence issues, they might be a bit withdrawn or depressed, as incontinence is linked to anxiety, depression, and the loss of independence.
But they don’t have to stress about having accidents. With the proper care, you can help your loved one confidently participate in their favorite activities while remaining comfortable and sanitary.
1. Have the right incontinence supplies. Getting incontinence products like adult briefs, pull-ons, underpads, or catheters will help your love one manage their leakage or other bladder issues successfully and comfortably.
2. Save on incontinence supplies through insurance. The monthly costs of catheter supplies, pull-ups, changing gloves, wipes, and more can quickly add up, becoming a stressful expense. But you don’t have to worry about it by qualifying to receive incontinence supplies through insurance. Best of all, we make the process easy!
3. Avoid bladder irritants. There are foods and beverages that can irritate your bladder, including:
- Spicy foods.
- Chocolate
- Fried foods.
- Greasy items.
- Coffee
- Sugary juices.
Avoid these items or only indulge in moderation to reduce incontinence symptoms. It’s much better to stick to organic juices, water, whole grains, fruits, and veggies to keep your system healthy and happy. Hydration will keep your juices flowing as fruits and veggies provide enough fiber to prevent constipation.
4. Prepare for accidents. Have a backpack with all the items you may need in the event of an accident. Have a change of clothes, wet wipes, disposal bag to mask smells and odors, as well as enough briefs or catheter supplies to last for the entire day.
5. Be supportive. Your loved one may have a difficult time facing incontinence, so offer them support and reassurance. Let them know that you’re there to help and confidently assist with managing their symptoms. Participate in their daily routines by making sure they’re prepared with their incontinence supplies and regularly go with them to the doctor to see about new incontinence procedures. While some patients with spinal cord injuries may have incontinence for the rest of their lives, others may be able to retrain their bladder over time.
How to Get Incontinence Products Through Insurance for Spinal Cord Injury
Continence care products, such as intermittent catheters, adult briefs, and protective underwear, can successfully manage incontinence if you have SCI. The products that are best suited for you will be based on your level of mobility and your specific injury, and you may be eligible to get them covered through your Medicaid or Medicare plan with Aeroflow Urology!
To see if you qualify for coverage, fill out our secure, 2-step Eligibility Form. Once you are eligible, we’ll reach out to your healthcare provider for a prescription on your behalf, and if you’d like to get your products even quicker, you can contact your provider’s office and let them know we’ll be requesting a prescription!
We’ll then ship your order in discreet boxes right to your doorstep for free. You can also refill your supplies monthly with our easy-to-use refill process.
Parittotokkaporn, S., et al. (2021). Transcutaneous Electrical Stimulation for Neurogenic Bladder Dysfunction Following Spinal Cord Injury: Meta-Analysis of Randomized Controlled Trials, Journal of the International Neuromodulation Society, 24(7), 1237-1246. DOI: 10.1111/ner.13459
The Neurogenic Bladder Research Group.(2015, December 31). Neurogenic bladder. Patient Information library. Retrieved from https://www.nbrg.org/articles?s=neurogenic-bladder
Spinal injury and Incontinence: What is the Link? (2018, August 28). Incontinence UK. https://www.incontinence.co.uk/spinal-injury-and-incontinence
Al Taweel, W., & Seyam, R. (2015). Neurogenic bladder in spinal cord injury patients. Research and Reports in Urology, 85. https://doi.org/10.2147/rru.s29644
Edited by Marlee Septak
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.