This piece has been medically reviewed by Susie Gronski, PT, DPT, Medical Advisor to Aeroflow Urology.
Functional incontinence can affect anyone, but it’s common for older adults and people with disabilities to experience it. Learn what causes this type of incontinence and use our 6 expert tips to help your loved one manage their symptoms.
What Is Functional Incontinence?
Urinary incontinence (UI) is the loss of bladder control and there are many different types of urinary incontinence people may experience, including:
- Stress incontinence: Leaking urine when sneezing, coughing, laughing, bending over, lifting heavy objects, or exercising.
- Urge incontinence: Also known as overactive bladder (OAB), feeling the strong and sudden urge to urinate, resulting in leakage, and using the bathroom more frequently than usual.
Check Your Eligibility
2 Easy Steps
From catheters to pediatric and adult incontinence supplies, discover the continence care essentials covered by your insurance.
- Overflow incontinence: Being unable to empty your bladder fully, resulting in leftover urine in the bladder which causes an involuntary loss of urine.
- Mixed incontinence: Experiencing one or more symptoms of two different types of UI (for example, urine leakage when coughing and urinating more than usual.
With functional incontinence, you may leak urine due to cognitive, physical, or environmental challenges.
How Does Functional Incontinence Affect Seniors & People With Disabilities?
Functional incontinence is common among seniors and people with disabilities. As people age, the bladder and pelvic floor muscles become weaker, causing loss of continence and may cause physical problems when using the toilet. People with disabilities, such as Alzheimer’s disease, may lose their ability to find or use the restroom.
Causes of Functional Incontinence:
- Arthritis
- Cerebral palsy (CP).
-
Neurological diseases, such as dementia, Parkinson’s disease, or Alzheimer’s disease.
-
Injuries (broken leg, etc.).
-
Multiple sclerosis (MS) or spinal cord injury (SCI).
-
Prostate cancer.
-
Poor vision or blindness.
- Certain medical conditions, like enlarged prostate in men.
- Weak bladder muscles or pelvic floor.
- Nerve damage that affects the bladder.
- Certain medications, such as diuretics.
A person with functional incontinence may:
- Have diminished cognitive or sensory awareness to urinate.
- Be unable to access a toilet.
- Have difficulty with taking clothes on and off.
- Have difficulty with mobility and transferring on and off the toilet.
- Have difficulty getting to the bathroom on time.
- Have diminished cognitive ability to recognize a bathroom or toilet.


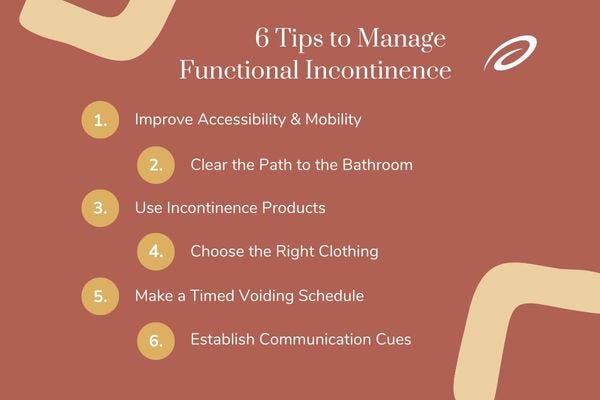
6 Tips to Manage Functional Incontinence
Functional incontinence may be reversible with modifications. Anything you can do for a loved one to improve their independence, accessibility, and function to use the toilet will improve their symptoms and help prevent accidents from occurring.
1. Improve Accessibility & Mobility
Improve accessibility & mobility around toileting. This might mean implementing bathroom modifications, such as raised toilet seats, grab bars, etc.
2. Clear the Path to the Bathroom
Remove clutter and potential fall hazards in the bathroom and the route to the bathroom. Make sure there is ample lighting in the bathroom and the route to the bathroom.
3. Use Incontinence Products
Incontinence products, such as adult briefs and protective underwear can help control leaks and keep your loved one dry and comfortable. If your loved one has a disability, they may qualify for free incontinence products every month.
4. Choose the Right Clothing
Make sure your loved one has clothing that’s easy to put on and take off (for example, if someone has dexterity difficulties with buttons, try an elastic waistband without buttons instead).
5. Make a Timed Voiding Schedule
Coordinate a timed voiding schedule so that you or your loved one can make it to the bathroom in time without feeling rushed.
6. Establish Communication Cues


If there are cognitive challenges present, establish a variety of communication cues to help your loved one recognize the toilet and find the bathroom. Be mindful of non-verbal cues that your loved one may need to use the bathroom.
Information provided on the Aeroflow Urology blog is not intended as a substitute to medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to continence care.