This piece has been medically reviewed by Aleece Fosnight, MPAS, PA-C, CSC-S, CSE, NCMP, IF, Medical Advisor to Aeroflow Urology.
It’s not surprising that seniors need to pay more attention to how they take care of their bodies due to the natural process of aging, but seniors also need to take extra care of their bladders and pelvic floors.
Senior citizens are more prone to bladder and pelvic floor issues, such as nocturnal enuresis (NE), weakened pelvic floor muscles, increased urinary frequency, functional incontinence, and stress incontinence.
Find out what you can do for yourself or a loved one to keep your urinary system healthy and strong to prevent these conditions from occurring.
Senior Bladder Problems
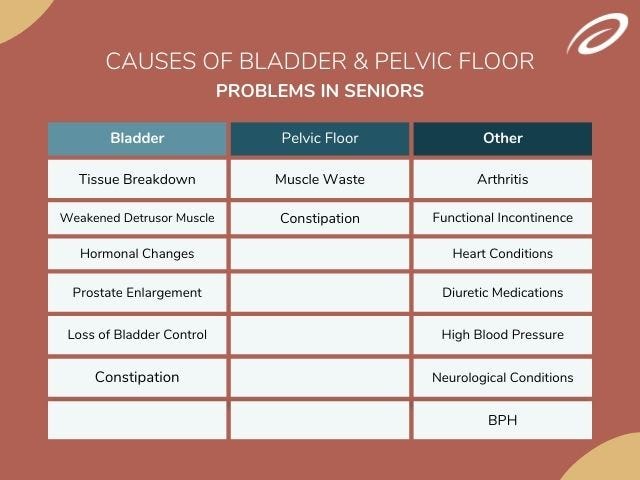
Seniors may experience bladder issues due to the following complications:
- Tissue breakdown. Senior bladders begin to wane in function secondary to tissue breakdown (muscle and nerve damage secondary to age and other comorbid conditions). This causes the bladder to decrease in compliance.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
- Weakened detrusor muscle. The detrusor (bladder) muscle weakens and the muscle does not squeeze as well to void the bladder, leading to retained urine and possible urinary tract infections (UTIs).
- Hormonal changes. Hormonal changes that occur during perimenopause and menopause cause certain urinary symptoms that are related to overactive bladder (OAB) / urge incontinence, stress incontinence, and increased risk of UTIs.
- Prostate enlargement. During the aging process, prostate enlargement can occur and this increases the pressure on the bladder, causing increased urinary urgency and frequency of the detrusor muscle. The prostate also narrows the urethra, causing a slower urinary stream and the detrusor muscle recognizes this, which causes the muscle to try and squeeze harder to void the bladder.
- Loss of bladder control. Similar to children ages 0-3 years old, seniors can lose control of their detrusor muscle due to the signaling to and from the micturition center declining with age. This is typically more significant for seniors over the age of 75.
- Constipation. Seniors who experience constipation may have urinary urgency due to the stool in the bowels pushing on the bladder, leaving less room for urine to fill and a more frequent need to urinate.
Senior Pelvic Floor Issues
Elderly people may experience pelvic floor issues that can be attributed to:
- Muscle waste. This occurs all over the body as we age and the pelvic floor muscles are not spared during this waste process. The pelvic floor muscles become weak and can lead to pelvic organ prolapse (POP). These muscles are one of the key components to bladder function and weak muscles can also lead to OAB, urinary frequency, and stress incontinence.
- Constipation. Constipation can cause pelvic floor dysfunction.
Other Factors That Cause Dysfunction
Other common factors can also cause bladder or pelvic floor dysfunction in seniors, including:
-
Arthritis. Arthritis causes inflammation in the body and this can be directly correlated with bladder function, as inflammation can increase irritation to the bladder leading to increased frequency.
However, most of the time, arthritis causes functional incontinence with difficulty transferring and pain, causing slower times getting to the restroom when a senior feels the need to void their bladder. If arthritis is occurring in the hands or wrists, this can lead to delays in removing clothing quickly enough to use the toilet.
- Functional incontinence. Transferring to a toilet and slower reaction times lead to increased functional incontinence in seniors more than any other age group. Functional incontinence in seniors is secondary to cognitive impairment and not having awareness of needing to empty their bladder.
- Heart conditions. Congestive heart failure is the most common cardiovascular condition that affects senior bladder function and incontinence. About half of all people with congestive heart failure have urinary incontinence.
- Diuretic medications. Medications that are taken by many seniors for issues, such as congestive heart failure, are diuretics. These medications are used to help relieve the extra fluid that builds up in the body for things to function optimally. They push fluids through the kidneys and into the bladder.


This increased volume of urine produced causes seniors to void more frequently and urgently.
- High blood pressure. High blood pressure is another heart condition that can affect the senior bladder. The medications for hypertension increase urine output and increase the number of times seniors use the restroom or need to void their bladders.
- Neurological conditions. Conditions such as Multiple sclerosis (MS), Parkinson’s disease, and Alzheimer’s lead to disruption of the signaling from the brain to the bladder, leading to overnight incontinence (NE).
- Benign prostatic hyperplasia (BPH). BPH is an anatomical change that can occur with aging. This condition can lead to overflow incontinence at night, prolapsed bladder, the inability to empty the bladder completely, and UTIs.
Understanding Incontinence
Incontinence is the term used to describe the loss of bladder or bowel control. Urinary incontinence (UI) is the loss of bladder control. There are many different types of UI that seniors (or any person of any age) can experience.
Stress incontinence (SI): Leaking urine when bending over, sneezing, coughing, laughing, exercising, having sex, or lifting heavy objects.
Overactive bladder (OAB) / Urge / Frequency incontinence: Feeling the sudden and frequent urge to urinate, resulting in urinating more than 8 times in 24 hours and more than 2 times overnight.
Overflow incontinence: Leaking or dribbling urine throughout the day due to the inability to empty your bladder fully.
Functional incontinence: Having control over your bladder but having accidents or leaks due to limited mobility of slow physical reactions.
Mixed incontinence: Experiencing two or more symptoms of one of the above types of incontinence at the same time.
8 Expert Care Tips
Unfortunately, our current medical society is more geared toward reactive and problem-focused concerns when it comes to preventing UI in seniors. However, with a more preventative, proactive approach, delay in bladder concerns and UI can be achieved.
If you’re helping an older loved one manage or prevent UI, or if you’re a senior looking to keep your bladder and pelvic floor muscles healthy, use these preventive care tips from our expert Medical Advisors.
1. Speak With a Healthcare Provider.
Talk to your healthcare professional about your concerns. Remember: UI can be common but it’s not normal. This can be the first step in improving bladder problems or pelvic floor dysfunction. Don’t be ashamed to speak with your provider about your symptoms.
UI is extremely common among people of all ages in the United States, especially among seniors. Speaking up will help destigmatize the shame we feel when discussing UI!


2. Use Adult Incontinence Products.
Adult incontinence products, such as adult briefs (adult diapers), adult protective underwear, and bladder control pads are excellent for controlling urine leaks throughout the day or night. Based on your level of leakage, certain products may be more suitable for you.
Adult briefs: For moderate to severe leakage.
Adult overnight briefs: Best suited for severe to overnight leaks.
Adult protective underwear: For light to moderate leakage.
Bladder control pads: Best for light leaks.
Did you know you may qualify to get free bladder control products through Aeroflow Urology? Find out if you qualify in under 5 minutes.
3. Work With a Pelvic Floor Physical Therapist (PFPT).
Working with a PFPT can help improve pelvic floor muscle function as well as balance and increase general strength to help you move better.
4. Increase Water Intake.
Drink more water throughout the day to keep your urinary system functioning properly, but limit fluids 2 hours before bed to reduce chances of accidents at night. And remember: While you may think decreasing fluid intake will reduce symptoms of UI, it actually can increase urinary urgency and frequency because dehydration produces more concentrated urine which irritates your bladder and makes you pee more!
5. Limit Certain Drinks.
Avoid caffeine after noon and limit alcohol intake, as these can both irritate your bladder- especially the senior bladder- and make symptoms of UI worse.
6. Avoid Constipation.
Eat a balanced diet with fiber, fresh vegetables, fruits, and fats (plus lots of water!) to keep things flowing since constipation can worsen symptoms of UI. Exercise also helps prevent constipation.
7. Stay Active.
Physical activity can improve bladder functionality and increase pelvic floor muscle strength. These activities can include things like:
- Stretching
- Walking
- Swimming
- Yoga
8. Control Comorbidities.
Controlling symptoms of other comorbidities to the best of your ability can optimize bladder and pelvic floor function and delay declines.
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.