When it comes to maintaining male well-being, there is one specialist who plays a crucial role in treating men’s needs – a urologist.
But, discussions surrounding men's health often tend to take a backseat, even in the male-provider relationship. However, just like women, men have specific health concerns that require attention and care from a urologist or pelvic floor specialist.
Throughout this article, we’ll explore the common urological conditions that affect men, including prostate health, erectile dysfunction, and urinary incontinence. We’ll discuss the role of urologists in addressing these issues and the available treatment options for such issues. Additionally, we’ll talk about the importance of seeing a urologist and shed light on the compelling reasons why men should prioritize this type of care.
What Is a Urologist?
A urologist is a healthcare provider who specializes in urinary health, male reproductive system problems such as male infertility, and beyond. Urologists treat a wide variety of conditions that can specifically affect men, but they can also treat women.
What Is a Pelvic Floor Therapist?
Check Your Eligibility
2 Easy Steps
From catheters to pediatric and adult incontinence supplies, discover the continence care essentials covered by your insurance.
When Should a Man See a Urologist?
Many men overlook the importance of seeking urological care until symptoms become overwhelming or sometimes debilitating. This might be because there is a common perception that urologists primarily treat female-identified patients. This perception may stem from the fact that conditions like urinary incontinence and pelvic organ prolapse are more commonly associated with women due to factors such as pregnancy and childbirth.
However, it's important to dispel this misconception and emphasize that urologists also play a crucial role in the care of men.
When you should see a urologist varies on you as an individual. Regular check-ups with a urologist may not be necessary for men without any specific symptoms or risk factors for urological or pelvic floor issues. Currently, there is no accepted consensus for the frequency of adult-male health examinations. However, regular urological check-ups may offer opportunities for appropriate screenings based on your age and medical history (such as prostate cancer screening), and address any specific concerns or symptoms you may have.
Our expert suggests that even if you don’t have pelvic or sexual health concerns, seeing a urologist or pelvic floor therapist can provide valuable pelvic and sexual health education. This type of education is not part of standard
Pelvic health physical or occupational therapy, also known as pelvic floor rehabilitation, is a form of medical therapy that focuses on improving the function of the pelvic floor muscles. These muscles support the bladder, rectum, and reproductive organs like the prostate.
The pelvic floor muscles play an important role in bladder and bowel control and sexual function. Factors like muscle tone, scar tissue, nerve injury, poor coordination and communication between muscles and nerves, nutrition, psychological and social factors can all impact pelvic and sexual health.
curricula in both early and young adult education. You should be aware of your sexual and pelvic health anatomy, and know what is normal so that you can recognize when to seek help if or when bothersome or problematic changes occur. Seeing a pelvic floor specialist or urologist can assist in this education.
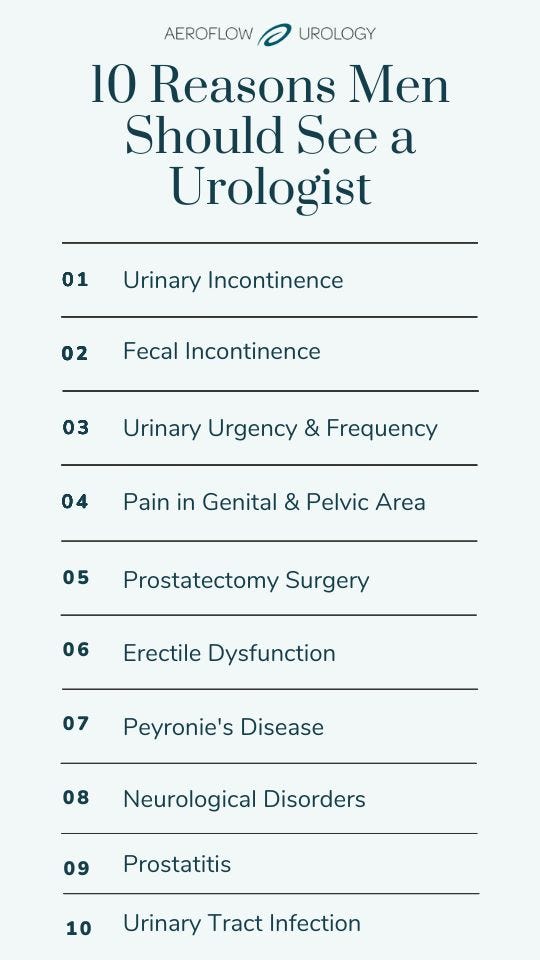
- Urinary incontinence
- Fecal incontinence
- Urinary urgency and frequency
- Pain in genital or pelvic area
- Pre and post-prostatectomy surgery (for incontinence and sexual recovery)
6. Erectile dysfunction
7. Peyronie’s disease
8. Neurological disorders
9. Prostatitis
10. Urinary tract infection
What Happens at a Man’s First Urology Visit?
Pelvic health specialists understand that discussing your pelvic and sexual health may be a sensitive and personal topic.
In your first session with a urologist or pelvic floor therapist, expect ample time to discuss your pelvic and sexual health concerns and urological problems, and address any questions or apprehensions you may have about the therapeutic process.
Your urologist may perform a physical exam to look for abnormalities or symptoms like enlarged prostate (benign prostatic hyperplasia or BPH). They may also perform a rectal exam, or check your testosterone levels if you’re experiencing male reproductive organ issues.
Some men have apprehensions around the internal pelvic muscle exam, and that’s okay. The good news is that an internal exam and treatment is not always necessary to feel better. Pelvic health specialists offer you multiple options to address your pelvic and sexual health concerns that aren’t intimidating.
In addition, due to the intimate nature of the pelvic health exam, physiological responses like an erection or spontaneous ejaculation may occur. Pelvic health therapists are equipped to handle these situations in a professional and compassionate manner. In some instances, spontaneous erections during an exam or treatment can be useful for diagnostic purposes like Peyronie’s Disease or painful erections.
You have permission to refrain from any part of the evaluation or treatments offered at any time during the course of your pelvic therapy care. Pelvic health specialists work collaboratively with you to set personalized health goals and develop a comprehensive plan that will help you restore healthy pelvic and sexual health function.
You have permission to refrain from any part of the evaluation or treatments offered at any time during the course of your pelvic therapy care. Pelvic health specialists work collaboratively with you to set personalized health goals and develop a comprehensive plan that will help you restore healthy pelvic and sexual health function.
Your urologist may also run tests to determine the cause of your issues. These tests may include:
- A quiz or survey for urinary incontinence.
- Urinalysis
- Urine culture.
- Bladder ultrasound.
Your specialist may also suggest different treatments for your condition at your first visit, as well as a follow-up appointment.


10 Reasons Men Should See a Urologist
1. Urinary Incontinence
Urinary incontinence is defined as a loss of bladder control. While it’s common among men, especially older men, it’s never normal. Two common types of urinary incontinence are stress urinary incontinence and urge urinary incontinence.
- Stress Urinary Incontinence: Involuntary loss of urine during physical and / or activities that cause exertion such as coughing, laughing, sneezing, lifting, and jumping.
- Urge Urinary Incontinence: Involuntary loss of urine following a sudden and strong urge to urinate.
2. Fecal Incontinence
Fecal incontinence is the experience of involuntary loss of stool with activity or following a sudden strong urge to have a bowel movement.
On occasion, you may experience diarrhea that makes it difficult to hold back stool and is typically not a cause for concern unless these symptoms are frequent, severe, or related to an illness. In these cases, seek medical consultation immediately, particularly from a gastrointestinal doctor. For fecal incontinence not related to illness, that is affecting a person’s quality of life, and causing emotional and social distress, it’s best to seek help from a pelvic health specialist.
3. Urinary Urgency & Frequency
Urinary urgency and frequency is a type of urinary incontinence. Symptoms include a strong urge to urinate that is difficult to defer, usually resulting in having to rush to find a bathroom. Symptoms also include voiding your bladder more than 6-8 times in a 24-hour period.
Experiencing urinary urgency from time to time is not problematic, but if it begins to disrupt your life (for example: always looking for a bathroom, avoiding activities you enjoy, or planning activities around a bathroom), it’s time to seek help from a pelvic health specialist.
4. Pain In Genital or Pelvic Area


Pain syndromes are often lumped under the umbrella of chronic pelvic pain syndrome (historically known as “chronic prostatitis” in men, but this term is outdated and its use is discouraged when describing / diagnosing pelvic pain in men that is not related to infection or local pathology).
Pain in your genital or pelvic area can include pain with:
- Erection
- Ejaculation
- Intercourse or anal sex
- Sitting
- Bowel movements.
- General groin pain, testicle pain, penis pain, etc.
Pain experienced during these activities or in these areas may be described as a deep ache, “golf ball” sensation in the rectum, sharp, burning, tightness, sore, or stabbing-like pain anywhere in the pelvic or genital region.
Other symptoms include:
- Lower urinary tract symptoms (urgency, frequency, incomplete emptying, urinary blockages, nocturia, incontinence, painful urination, difficulty voiding or trouble urinating).
- Digestive pain (constipation, nausea, bloating, incomplete emptying).
- Changes in sexual function (ED, PE, decreased sexual desire).
- Mood changes (anxiety, depression, worry, frustration, anger).
It’s important to note that while occasionally feeling a bit of pain in the pelvis is not cause for concern, persistent symptoms that affect your quality of life or cause emotional and social distress is not normal. If symptoms persist or get worse for more than a few days, you should seek immediate help from a urologist to initially rule out infections or other potential medical causes. After ruling out infectious disease and local pathology, you should immediately see a pelvic health specialist to get help and support for their pelvic and sexual pain concerns.
5. Pre & Post-Prostatectomy Surgery
You may require prostatectomy surgery if you have prostate issues. Symptoms that occur after prostatectomy surgery may include:
- Urinary incontinence.
- Erectile dysfunction.
- Pain
While we don’t have evidence of exactly when post surgery you should seek care from a pelvic health specialist, we do know that pelvic therapy can help with incontinence and sexual recovery after prostatectomy surgery. There is also evidence that shows working with a pelvic floor specialist prior to prostate surgery can improve bladder control and sexual recovery outcomes post-surgery.
6. Erectile Dysfunction


Erectile dysfunction (ED) occurs when you can’t achieve or maintain an erection. The main symptom of ED is the recurrent inability to obtain or maintain an erection sufficient for sexual activity (mostly defined in terms of intercourse) lasting greater than 3 months.
It’s common for men 55 years old and younger to experience at least 1 episode of erectile failure. It’s also normal for erections to wax and wane during sex. But, if these symptoms become persistent, consistent, or cause emotional and social distress, you should seek help from both a urologist (to rule out physical causes like cardiovascular disease, diabetes, or medication-induced ED), a pelvic health specialist, and a sex therapist.
7. Peyronie’s Disease
Peyronie’s disease is a disorder where plaque forms under the skin of the penis. This plaque typically builds up inside the penis but can occur anywhere along it. This plaque build-up causes penile deformity.
Symptoms may include:
- Penile pain.
- Curvature, hinging, narrowing, or shortening of the penis when in an erect state.
Penises come in all shapes and sizes but if these symptoms / penile changes are different for you, and are causing pain or discomfort with sex for you or your partner, you should seek medical consult from urologist (they can do a penile doppler scan to determine if it is Peyronie’s disease). You should also seek care from a pelvic health specialist because there are conservative treatment options available to reduce symptoms and get back to pain-free sex!
8. Neurological Disorders
Neurological disorders, such as Parkinson’s disease, spinal cord injury (SCI), spina bifida, or multiple sclerosis (MS), can cause urinary and sexual health problems in men. Symptoms are highly variable based on the complexity of your health concerns. Some symptoms may include:
- Urinary incontinence,
- Urinary retention.
- ED
- Difficulty ejaculating, or ejaculatory control issues.
- Difficulty orgasming.
- General mobility and functional limitations that impact the ability to participate in sexual activities.
There is no guidance around timeframes of when you should seek care from a pelvic health specialist,


but we believe a pelvic health specialist should be part of your care team at the onset of your diagnosis of these conditions, and certainly at any point along your health journey.
-
Transcutaneous electrical nerve stimulation (TENS): A type of electrical stimulation that is commonly used to treat pain. More recently there is some literature available around the use of TENS for the treatment of overactive bladder symptoms. The exact mechanisms of transcutaneous electrical nerve stimulation (TENS) is still unclear. It has been postulated to work by reorganization of spinal reflexes and regulation of cortical activity, stimulation of sensory nerves that communicate with the micturition centers via sacral nerve roots.
-
Pelvic floor muscle assessment and treatment with a pelvic therapist.
-
Dietary changes: Avoiding bowel and bladder irritants, such as alcohol, caffeine, soda, spicy foods, tomato-based products, etc.
- Bladder control products: Wearing male incontinence products, like men’s protective underwear or adult briefs, may help to alleviate symptoms of urinary incontinence while you seek treatment to reverse your symptoms. You may be able to get male bladder care products for free through your insurance plan!
- EMG biofeedback: Electromyography that involves sensors (rectal, vaginal, or external electrodes on perineum) that feed back muscle activity data to a machine which then offers visual feedback to the person. These sensors read muscle electrical activity not strength. Biofeedback, whether tactile, visual, pressure or electromyography is used to help people feel more confident and capable with doing their pelvic floor exercises.


9. Prostatitis
Prostatitis is an infection of the prostate or inflammation of the prostate.
Different types of prostatitis are:
- Acute bacterial prostatitis.
- Chronic prostatitis.
- Chronic bacterial prostatitis.
- Pelvic pain syndrome.
This is a painful condition and can display symptoms such as:
- Fever
- Pain in the bladder, rectum, or lower back.
- Pain or burning when voiding the bladder or ejaculating.
- Feeling like you have a full bladder all the time
- Blood in your semen
- Split urine stream
If you have any of these symptoms, you should see a urologist to be properly diagnosed and treated.
10. Urinary Tract Infection
A urinary tract infection (UTI) occurs when your urinary system (bladder, urethra, kidneys) becomes infected with bacteria. UTIs are caused when bacteria from the anal or genital areas travel from the urethra into the bladder.
Symptoms of a UTI include:
- Pain or burning sensation with urination.
- Abdominal cramps.
- Frequent urination or a constant urge to urinate.
- Releasing small amounts of urine at a time (urinary retention).
- Cloudy or bloody urine.
- Fatigue or dizziness.
- Fever, chills, or nausea (this may indicate that the infection has reached the kidneys).
If you have symptoms of a UTI, you should seek attention from a healthcare provider or urologist. Your provider will likely collect a urine sample to confirm the presence of bacteria and determine other risk factors. You’ll then likely receive a course of antibiotics to treat the infection.
Possible Treatments From a Urologist
If you are diagnosed by your urologist or pelvic floor specialist with any conditions that may cause problems, your provider may recommend the following treatments. The treatments you receive will vary on your diagnosis and individual treatment plan.
- Bladder retraining: This technique involves establishing a regular schedule for bladder voiding using techniques to help improve control. It may be combined with dietary modifications and medications.
- Functional training strategies for incontinence that is caused by cognitive, mobility or dexterity issues that impact continence control:
-
- Environmental modifications.
- Clothing adaptations.
- Continence support devices.
- Caregiver training.
- Lifestyle coaching: Changes in exercise, diet, sleep, and smoking cessation.
- Collagen injections: Collagen-like material can be injected into the bladder neck to help increase bulk of tissues and help with continence control.
- Medications that help relax the bladder (i.e, for bladder spasms, overactive bladder), medications to reduce digestive side effects for constipation, or medications for bacterial infection.
The Importance of Men’s Urological Health
While speaking about urological issues may be difficult at first, it’s imperative to speak with your primary care provider and specialists to assess and treat your health issues. Prioritize your well-being and help break down stigmas surrounding urological conditions by openly discussing dialogue. Doing so can make a significant difference in your life and quality of life!
References
Milios, J. E., Ackland, T. R., & Green, D. J. (2019). Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urology, 19(1). https://doi.org/10.1186/s12894-019-0546-5
Penile Curvature (Peyronie’s Disease) - NIDDK. (n.d.). National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved May 23, 2023, from http://niddk.nih.gov/health-information/urologic-diseases/penile-curvature-peyronies-disease#:~:text=Peyronie
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.