Key Takeaways:
-
Pelvic pain and incontinence are common—but not normal—and you deserve real answers and care.
-
Recent studies show that some women's pelvic pain symptoms are dismissed by their providers.
-
Learn how to advocate for yourself and get women's incontinence supplies covered through insurance.
Many women face a challenging reality: Managing pelvic pain and urinary incontinence while feeling ignored by their healthcare providers.
Pelvic pain and urinary incontinence are common issues, affecting over 60% of women– specifically up to 25% of reproductive-aged women.
Yet, symptoms of pelvic pain symptoms reported to providers are often downplayed or dismissed. Being told to "try to relax" or that pain is "stress-related" is unfortunately common, according to a recent study.
This article will offer support, understanding, and credible information, so you can identify your symptoms and advocate for yourself with your provider. We’ll also tell you how to get free women’s incontinence supplies through insurance so you can manage your leakage with confidence.
Normalizing Women's Pelvic Pain
Women have historically faced barriers when seeking solutions to their health issues, whether due to societal misconceptions or the medical normalization of their pain and symptoms—underplaying and misunderstanding postpartum incontinence and endometriosis are great examples of this.
One common misconception is that urinary incontinence and pelvic pain are simply normal parts of life for women, especially during pregnancy, after vaginal delivery, or in menopause. Many women are familiar with the old saying, “Pain is a natural part of being a woman.” However, this is not the case at all.
Just because something is common does not mean that it is normal. Pelvic pain and incontinence deserve serious attention, thorough investigation, and prompt treatment.
Unfortunately, the historic normalization of women’s pelvic pain and bladder symptoms—whether internalized by women, perpetuated by societal norms, or reinforced by their healthcare providers—has created mental and physical challenges. As a result, many women delay or avoid seeking proper care because they believe their symptoms aren’t “bad enough.”
Dismantling this bias is the first step toward empowering women to take control of their pelvic health.
Pelvic Pain & Urinary Incontinence Explained
Understanding pelvic pain and incontinence is essential for identifying your symptoms and seeking care.
Urinary Incontinence
Urinary incontinence is the unintentional loss of urine, with symptoms ranging based on the type of incontinence you have.
- Stress incontinence: Leaking urine during physical activities like coughing, sneezing, or exercising.
- Urge incontinence: Feeling a sudden, intense urge to urinate followed by involuntary leakage.
Other types of incontinence exist, and sometimes different types occur at the same time (mixed incontinence). Understanding these can help you communicate with your provider about the type you are experiencing.
Pelvic Pain
Pelvic pain is discomfort experienced below your belly button, extending to the upper thighs. Symptoms can vary from person to person. It may be described as constant and severe, a dull ache, sharp pains, cramping, or a sensation of pressure.
Pelvic pain can develop from a variety of gynecological and non-gynecological factors. Common causes include:
- Endometriosis
- Ovarian cysts.
- Pelvic inflammatory disease.
- Pelvic floor muscle dysfunction.
- Urinary tract infections.
- Interstitial cystitis.
- Underlying symptoms, such as irritable bowel syndrome (IBS).
In some cases, urinary incontinence and pelvic pain are connected, with pelvic floor dysfunction being a contributing factor to both, which is why it's essential to speak with an understanding healthcare provider about your symptoms.
Common but Not Normal
While these conditions may be prevalent among women, it's crucial to understand that incontinence and pelvic pain are not normal and are not symptoms you have to endure without treatment.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Why It's Important to Advocate for Yourself
If you don't advocate for yourself in your visit with your healthcare provider, you may face the following issues:
Delayed or Missed Diagnoses & Worsening Conditions
Some of the biggest impacts not advocating for yourself can have is delayed or missed diagnoses. Leaving pelvic pain or incontinence undiagnosed can leave conditions, like endometriosis, interstitial cystitis, incontinence, or pelvic floor disorders untreated, allowing them to progress and possibly lead to increased pain, complications, reduced quality of life, and irreversible damage.
Financial & Time Strains
Seeking out medical care sometimes involves visiting multiple providers, especially when you are dismissed and walk away without a proper diagnosis or treatment. This can take time away from your work hours or other activities and responsibilities. It can also result in paying more for medical visits, causing financial strain.
Lack of Self-Advocacy
Feeling unheard by your healthcare provider may make it harder to speak up during future visits. This can lessen your self-confidence and your ability to advocate for yourself.
A Woman's Guide to Self-Advocacy
While systemic changes are needed, proactive strategies can improve your healthcare experiences. Self-advocacy is an essential skill you need to develop so your medical needs are met and treated.
Trust Your Body
You must remember to trust yourself and your instincts. You are the expert on your body. If you're experiencing symptoms of incontinence or pelvic discomfort, validate yourself and seek out a provider who will listen to your concerns.
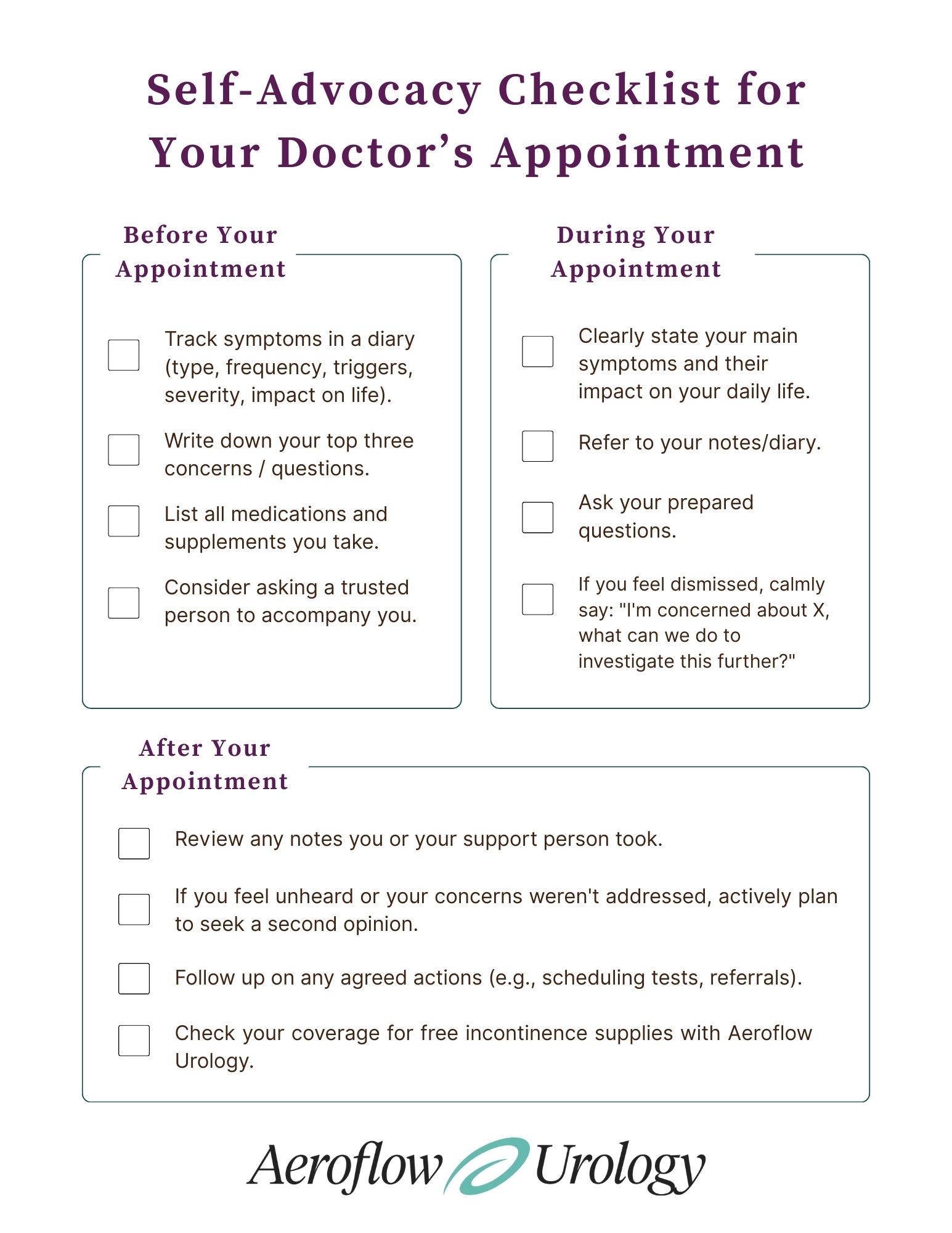
Prepare for Your Appointments
Preparing to talk with your provider about incontinence or pelvic symptoms you may feel are embarrassing can be tough. However, ensuring that you're ready for your visit can help.
- Use a bladder or symptom diary: Detail symptoms, timing, frequency, triggers, severity, and impact on your daily life. This gives your provider concrete proof of your symptoms. A diary may also help your physician more quickly identify which type of condition you may have.
- Take a list of questions: Write down questions about your symptoms before your appointment to ensure you cover everything that’s important to you. You can also download Aeroflow Urology's list of questions to ask your provider and take it with you.
- Prepare a medical history summary: Before your appointment, gather what you can of your medical history, current / past medications, and past treatments. This will help your provider understand your medical background and make the treatment process smoother.
Be Calm, Clear, & Assertive!
How you communicate with your provider may be key to receiving proper diagnosis and treatment.
- Use clear, specific language about symptoms and their impact on your daily life.
- Don't hesitate to express concerns or ask for clarification.
- If you feel dismissed, let your provider know you need them to take your symptoms seriously.
- Ask your provider to document your concerns in your chart for future reference, whether with your current or future physician.
Get a Second or Third Opinion
You are not obligated to stay with a provider who isn't listening. Seeking a second or third opinion is acceptable and often necessary to find supportive care if you aren't being heard.
Finding Specialists Who Understand Women's Pelvic Health
Finding a provider who understands and treats pelvic pain and incontinence is critical. If you have persistent or complex symptoms, you may require a specialist. Specialists include:
- Urogynecologist: Specializes in female pelvic medicine and reconstructive surgery for pelvic floor disorders, such as incontinence and prolapse.
- Urologist: Specializes in urinary system disorders in women (and men), treating incontinence and bladder issues.
- Pelvic Floor Physical Therapist (PFPT): Trained to evaluate and treat pelvic floor muscle dysfunction, a contributor to pain and incontinence, using exercises, manual therapy, and biofeedback.
- Gynecologist with a Special Interest: Some OB-GYNs focus on chronic pelvic pain or endometriosis.
- Pain Specialist: May be beneficial for nerve-related pelvic pain.
What to Look For In a Healthcare Provider
Beyond credentials, look for someone who:
- Listens attentively and validates your experience.
- Asks thorough questions and looks into your concerns.
- Explains information clearly and encourages shared decision-making.
- Makes you feel comfortable and safe.
- Is willing to give you a referral when needed.
Get Free Incontinence Support With Aeroflow Urology
Aeroflow Urology's philosophy is rooted in empathy, education, and providing practical solutions to empower individuals to manage incontinence with dignity and confidence.
Support & Resources for Women
- High-quality incontinence supplies: You may qualify for free women's incontinence supplies, such as discreet pads and protective underwear for comfort and leakage management.
- Insurance coverage assistance: We help determine if insurance (including Medicaid) covers supplies and handle the paperwork for you. Check your coverage with Aeroflow Urology's simple Eligibility Form and let us handle the rest.
- Educational blog content: We consistently publish medically-reviewed articles by our trusted staff and Medical Advisors on urological conditions and management.
Managing pelvic health issues and gaslighting is challenging, but there is hope! Improvements in your symptoms and pain are possible with the correct information, support, and self-advocacy.
You deserve to be heard, validated, and receive compassionate care. It's never too late to seek the right kind of help.
References:
Patel, U. J., Godecker, A. L., Giles, D. L., & Brown, H. W. (2022). Updated Prevalence of Urinary Incontinence in Women: 2015–2018 National Population-Based Survey Data. Female Pelvic Medicine & Reconstructive Surgery, 28(4), 181–187. https://doi.org/10.1097/spv.0000000000001127
Moss, C., G Skovronsky, Holloway, J., Lorenzini, S., I Kopits, Rieff, M., Mitchell, L., Krapf, J., C Pukall, & Goldstein, A. (2024). (086) MEDICAL GASLIGHTING AND VULVOVAGINAL PAIN DISORDERS. The Journal of Sexual Medicine, 21(Supplement_5). https://doi.org/10.1093/jsxmed/qdae054.081
Pelvic Pain in Women: Misunderstood and Underreported, but For How Long? (2025, January 22). Stanford Pain News; Stanford University. https://painnews.stanford.edu/news/pelvic-pain-women-misunderstood-and-underreported-how-long
Garner, G. (2024, July 19). Medical Gaslighting: What It Is and What To Do About It - Garner Pelvic Health. Garner Pelvic Health. https://garnerpelvichealth.com/medical-gaslighting-what-it-is-and-what-to-do-about-it/
What is causing my pelvic pain, and when should I seek help? (2024, November 5). Nebraskamed.com; Nebraska Medicine. https://www.nebraskamed.com/health/conditions-and-services/womens-health/what-is-causing-my-pelvic-pain-and-when-should-i-seek
Hintz, E. (2025, May 8). When doctors don't believe their patients' pain – experts explain the all-too-common experience of medical gaslighting. SFGATE; Associated Press. https://www.sfgate.com/news/article/when-doctors-don-t-believe-their-patients-20316969.php
Corcione, A. (2025, April 24). These Stats on Medical Gaslighting & Pelvic Pain Are Unacceptable. Theoriginway.com. https://www.theoriginway.com/blog/shocking-stats-on-medical-gaslighting-pelvic-pain
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.