Key Takeaways:
- Increased progesterone levels cause the bladder to contract more often and cause the body to release more fluid, leading to incontinence.
- Low estrogen levels during menstruation change abdominal pressure, leading to weakened urethra and pelvic floor muscles, causing incontinence.
- Period products change abdominal pressure, causing incontinence.
From bloating to painful cramps to breakouts, many inconvenient symptoms accompany your period, but did you know incontinence may be another symptom?
This post will address why you may be experiencing incontinence during menstruation— a condition known as cyclical incontinence—and what you can do to help ease your symptoms.
What Is Urinary Incontinence?
Urinary incontinence is described as the loss of bladder control. There are a few types of urinary incontinence:
Stress incontinence: Stress urinary incontinence (SUI) occurs when abdominal pressure is placed on your bladder when you sneeze, cough, laugh, or engage in physical activities, such as exercising or heavy lifting. The pressure put on your bladder during these activities causes leakage.
Overactive bladder (OAB): You may be able to tell if you have an overactive bladder if you feel the need to urinate more frequently than usual (more than 8 times a day).
You may also feel the need to wake up in the night to pee.
Urge incontinence: Urge incontinence is when you feel the need to urinate frequently and urgently. Urge incontinence usually leads to urine leakage if you can’t make it to the bathroom on time or if your pelvic floor muscles or urethral sphincter are weak.
Overflow incontinence: Overflow incontinence occurs when your bladder doesn’t empty completely. When you have overflow incontinence, urine leaks or dribbles from your bladder.
Mixed incontinence: Mixed incontinence occurs when you experience multiple types of incontinence at once. Symptoms are based on what kind of incontinence you are managing.
Incontinence can be a lot to manage, especially if you’re experiencing premenstrual symptoms or menstrual symptoms at the same time.
Your Period & Hormones
Your body releases 4 different hormones, all in the name of reproduction. These hormones work together to regulate your period. Let's discuss 2 of the main hormones that can affect your bladder: Progesterone and estrogen.
Progesterone is a hormone released by your ovaries during your menstrual cycle. Its primary function is to prepare your body for pregnancy in case an egg is fertilized during ovulation. During this time, progesterone levels rise for about 5 days.
Estrogen is the hormone that maintains your reproductive and sexual health. This hormone is why women have periods, can get pregnant, experience menopause, and have breasts and wide hips. Estrogen is released in your body before and during ovulation, and thickens the uterine lining to prepare the uterus ready for pregnancy.
The menstrual cycle releases these hormones during 3 stages:
- Follicular stage: This is the stage before your egg is released. During this stage, levels of estrogen and progesterone are low.
- Ovulatory stage: In the ovulatory stage, your body releases an egg for fertilization, your estrogen levels drop, and progesterone increases.
- Luteal stage: This stage occurs after your egg is released. During the luteal phase, your progesterone and estrogen levels are high.
The fluctuation of progesterone and estrogen is why you experience symptoms during your cycle and while on your period. Most women experience premenstrual syndrome (PMS) about 1-2 weeks before bleeding begins.
What Causes Urinary Incontinence During Your Period?
So, why does incontinence happen during your period? Well, while there isn’t much urodynamic research to explain the relationship between menstrual cycles and urinary incontinence, there is a prevalence of incontinence symptoms during women’s periods.
On top of women reporting incontinence symptoms during their cycles, new studies are digging deeper into the effects the menstrual cycle has on the bladder.
1. High Progesterone
One study found that it’s common for women to experience incontinence during their periods.
The study included 133 pre-menopausal women with regular periods who were not taking hormones. Out of the 133 women, 41% reported experiencing incontinence at different times during their periods.
- 42% found incontinence was worse right before their period.
- 36% found incontinence was worse during their period.
- 15% found incontinence to be worse in the middle of the month.
- 7% found incontinence to be worse immediately after their period.
The study also reported that women were experiencing noticeably increased activity in their detrusor muscle following ovulation.
The detrusor muscle lines your bladder and squeezes inward when you pee, helping to push urine out the bladder through the urethra. If the detrusor muscle’s activity increases or is unstable, it can cause incontinence symptoms (e.g., the sudden urge to pee or frequent urination) linked to urge incontinence, SUI, overflow incontinence, and OAB. Because we know progesterone levels increase after ovulation, it’s suggested that these high levels of the hormone may cause an uptick in detrusor activity.
Another study that used detrusor tissue and progesterone found that progesterone levels did, in fact, directly affect detrusor muscle contractions.
Progesterone also tells your body to let go of all the fluid it held onto during your period, including urine. When this happens, you may feel the need to void more frequently, which is the main symptom of OAB.
Takeaway: If progesterone levels are going up during and after your cycle, and progesterone causes your bladder to contract more frequently, it may cause incontinence. Progesterone also causes your body to release fluid, leading to symptoms related to OAB.
2. Low Estrogen Levels
We know that estrogen plays a huge role in women’s health. It is the reason for your period, pregnancy (if you decide that’s right for you), and menopause. It’s why you may look different from a male. Basically, estrogen controls a lot of what happens in the female body.
Not only is estrogen released throughout your menstrual cycle, but our pelvic organs and pelvic tissues are also responsive to the hormone. This means that those parts of your body change as the levels of estrogen change.
Low estrogen levels cause a change in abdominal pressure, making the pelvic floor muscles and ligaments surrounding your pelvic floor to decrease in strength and increase in stiffness, which may lead to pelvic floor disorders and different types of incontinence.
Estrogen levels can also change the positioning of your cervix, which directly affects the strength of your sphincter and urethra. These change can make it challenging to void your bladder and stop urine from leaking out.
Takeaway: The low estrogen levels during menstruation alter abdominal pressure, causing your urethra and pelvic floor muscles to weaken, leading to incontinence.
3. Using Period Products
Hormones aside, there’s one other suspect that could cause incontinence during your period: Period products! When you put a tampon in your vagina, you change the pressure inside your abdomen.
This change in pressure can make your bladder muscles tighten or loosen, leading to incontinence symptoms, such as urinary retention and leakage.
Leakage while using a tampon may also be a sign of bladder prolapse, also known as a cystocele. Cystoceles can occur after childbirth, constipation, lifting heavy objects, chronic coughing, or pressure on the pelvic muscles. When you have a cystocele, the walls between your bladder and vaginal wall are weakened and cause your urethra to “kink.” This can block the urine from flowing out properly.
Still, when you use a tampon, it can do what a vaginal pessary usually does (more about that below) and open the urethra to allow urine to flow, leading to leakage.
Takeaway: Menstrual products, like tampons, can cause changes in your abdominal pressure, causing urinary retention and leakage. Tampons can also cause leakage by unknowingly fixing a pre-existing urine flow issue.
Tips to Manage Urinary Incontinence
If you’re experiencing incontinence during your period or your cycle, it can change your quality of life. But don’t worry—there are many treatment options available. You can speak with a healthcare professional, like your gynecologist or pelvic floor physical therapist, about a treatment plan or try out some simple at-home treatments.
1. Pelvic Floor Exercises
Also known as Kegel exercises, these exercises can help improve the strength of your pelvic floor. Even if you don’t have incontinence, you should do pelvic floor exercises to help keep your pelvic area strong and continent.
2. Incontinence Products
If you find that you’re leaking through your clothes or just want help managing your incontinence, incontinence products may be the answer. Protective adult underwear or bladder pads can help absorb leaks and keep you dry and worry-free. Find out if you qualify to receive incontinence supplies free through your insurance at the bottom of the page.
3. Lifestyle Changes
Making specific lifestyle changes may help you manage your incontinence. Drinking lots of water, eating healthy foods, exercising, and avoiding bladder irritants like caffeine, alcohol, and certain spices can all help improve incontinence symptoms.
4. Medications & Surgeries
Speak with your healthcare professional about which medicines may be able to help treat incontinence symptoms, or talk to your provider about bladder Botox injections or vaginal pessaries.
5. Weight Management
Maintaining a healthy weight is helpful when managing incontinence symptoms since excess weight can put pressure on your bladder and increase incontinence symptoms. Therefore, aim for a healthy amount of weight loss and exercise to keep your incontinence in control.
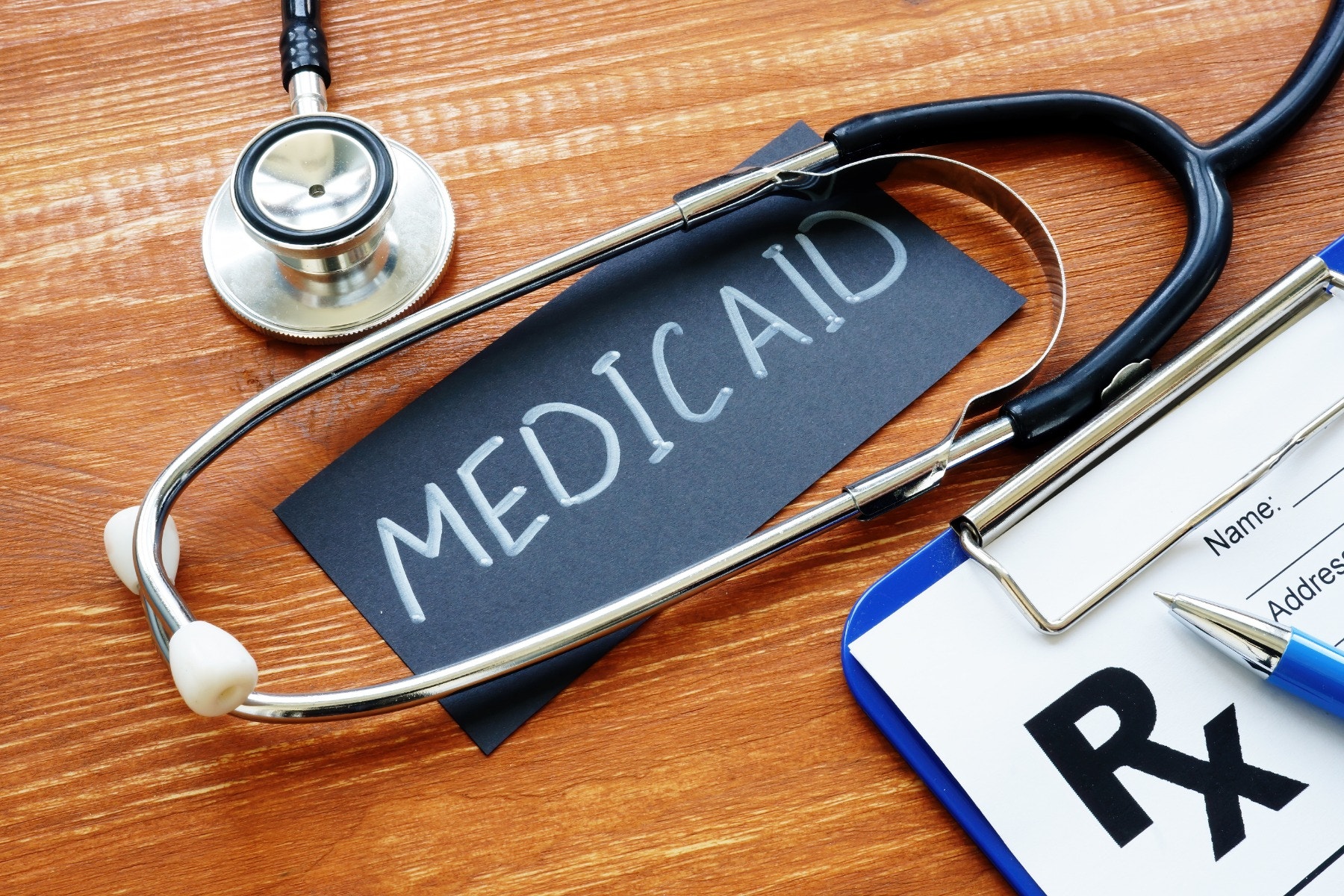
Qualifying for Free Urinary Incontinence Products
Aeroflow Urology knows managing incontinence symptoms can be difficult at times, especially if you’re also managing symptoms of menstruation. Let us do the work for you regarding incontinence care by sending you free incontinence supplies every month if you qualify.
If you have a pre-existing condition that causes urinary incontinence, Aeroflow Urology, along with your Medicaid-managed care plan, may be able to help. Here’s how it works:
Step 1. Fill out our Eligibility Form.
Step 2. Once you’ve submitted the form, one of our Continence Care Specialists will reach out to let you know if you’re eligible. From there, we’ll guide you through our products and give you a curated shopping list to choose your incontinence supplies from. Our specialists will help you select the perfect products for you.
Step 3. After choosing your products, they’ll be shipped directly to your door in discreet packaging. We’ll send you email or text reminders each month to let you know when it’s time to resupply.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
Progesterone - Health Encyclopedia - University of Rochester Medical Center. (n.d.). Www.urmc.rochester.edu. Retrieved April 7, 2022, from https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=167&ContentID=progesterone#:~:text=After%20ovulation%2C%20progesterone%20levels%20go
Hextall, A., Bidmead, J., Cardozo, L., & Hooper, R. (2001). The impact of the menstrual cycle on urinary symptoms and the results of urodynamic investigation. BJOG: An International Journal of Obstetrics and Gynaecology, 108(11), 1193–1196. https://doi.org/10.1111/j.1471-0528.2003.00280.x
Shenfeld, O. Z., McCammon, K. A., Blackmore, P. F., & Ratz, P. H. (1999). Rapid effects of estrogen and progesterone on tone and spontaneous rhythmic contractions of the rabbit bladder. Urological Research, 27(5), 386–392. https://doi.org/10.1007/s002400050168
Menstrual Cycle - Women’s Health Issues. (n.d.). Merck Manuals Consumer Version. Retrieved April 7, 2022, from https://www.merckmanuals.com/home/women-s-health-issues/biology-of-the-female-reproductive-system/menstrual-cycle#:~:text=Luteinizing%20hormone%20and%20follicle%2Dstimulating
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.