Key Takeaways:
- Gender-affirming surgery is a crucial step in aligning physical appearance with gender identity, but it's important to address potential challenges like urinary incontinence afterward.
- Both MTF and FTM surgeries can lead to urinary incontinence, manifesting in symptoms like weak urine flow and urinary tract infections.
- Treatment options include toileting techniques, incontinence products, collagen injections or pelvic floor therapy, dietary changes, and knowing your healthcare rights for proper care.
Undergoing gender-affirming surgery is a life-changing decision for those seeking to align their physical bodies with their gender identity.
This surgery can be a milestone in an individual’s journey towards self-acceptance, and while the positive outcomes of gender-affirming surgery are widely recognized health care community, it’s crucial to address the physical and emotional challenges that can arise after surgery is performed.
In this article, we’ll talk about the types of gender-affirming surgeries and the side effects they can have on your urinary system and mental health, as well as treatments that are available for those with urinary incontinence.
What Is Gender-Affirming Surgery?
Gender-affirming surgery, also called sex reassignment surgery or gender confirmation surgery, is a procedure that helps individuals “transition to their self-identified gender.” Gender-affirming surgery is elective and is not required to affirm someone’s self-identified gender, but many individuals choose to undergo it.
Check Your Eligibility
In Under 2 Minutes
Discover the incontinence products available through your insurance plan.
In many cases, quality of life has been shown to improve after undergoing gender-affirming surgery. One recent report that combined 27 studies of 2,718 cases of gender-affirming surgery showed that transwomen and transmen reported more satisfaction with their bodies, as well as a higher quality of life after the surgery was completed. However, it was also reported that mental health issues and mortality remained higher than cisgender individuals (people whose bodies align with their gender identity).
Types of Gender-Affirmation Surgeries
There are many different types of plastic surgeries a transgender patient can choose to undergo from a healthcare provider depending on which gender they identify with. These surgical procedures can be for female-to-male (FTM) or male-to-female (MTF) surgeries.
As with any surgical procedure, there are risks, and it is important to consult with your healthcare provider on any questions you have about potential complications. It should also be noted that not all transgender people choose to, or can afford to, undergo the medical procedures listed below, and this is perfectly fine.
Transmen Surgeries
Transgender men have several options when it comes to surgically affirm their gender identity. Two of the procedures, often referred to as “bottom surgeries,” are metoidioplasty and phalloplasty.
Metoidioplasties and phalloplasties are surgical procedures by which a penis is constructed.
- Metoidioplasty: A procedure that involves changing the clitoris into a penis. During this procedure, the surgeon will also perform a vaginectomy, removing the vagina. This procedure is different from a phalloplasty in that it only creates a micropenis and will not enable the individual to stand while urinating.


- Masculinizing phalloplasty: A procedure in which grafted skin (often from the thigh or arm) is used to construct a neopenis. A lengthening of the urethra is required to allow for urination through the neopenis. Potential complications with phalloplasties are the development of urinary stenosis or fistulas, which can increase the risk for urinary tract infections (UTIs), as well as the possibility that an intermittent catheter will be required to keep the urethra intact
- Facial reconstructive surgery: (Facial feminization surgery or facial masculinization surgery) Makes facial features more masculine or feminine.
Transwomen Surgeries
When making the decision to undergo a gender-affirming surgical procedure, transgender women may elect to undergo a procedure that shortens their urethra. These procedures include vaginoplasty, top surgery, and thyrochondroplasty.
- Feminizing vaginoplasty: Sometimes called "bottom surgery" or genital surgery, creates female genitalia, such as the clitoris, labia, and vagina.
- Chest surgery: Also called “top surgery,” breast augmentation, or chest reconstruction, removes or resizes breast tissue to create more masculine or feminine chest features.
- Reduction thyrochondroplasty: Reduces the size of the adam’s apple for more feminine features.
- Facial reconstructive surgery: (Facial feminization surgery or facial masculinization surgery) Makes facial features more masculine or feminine.
Other therapies that can be given to transgender persons are hormone therapy and voice therapy.
What Is Urinary Incontinence?
Urinary incontinence (UI) is the loss of bladder control that results in an involuntary loss of urine. UI can occur in any person of any age and develops for many different reasons, including surgical treatment.
Stress incontinence: Stress urinary incontinence results in leaking urine when running, jumping, laughing, sneezing, coughing, or lifting.
Overactive bladder (OAB) / Urge incontinence: Voiding the bladder more than 8 times in a 24-hour period, or feeling the intense and sudden urge to urinate, resulting in leakage.
Overflow incontinence: Frequent or constant dribbling of urine due to the inability to empty the bladder completely.
Functional incontinence: Urine leaks due to limited mobility or neurological disorders, such as Parkinson’s disease.
Mixed incontinence: Experiencing 2 or more types of UI symptoms at once, such as stress incontinence and OAB.
UI, though not experienced by all people, can impact both physical and emotional well-being after gender-affirming surgery is performed. The symptoms experienced can range from occasional to severe leakage that may require treatment.
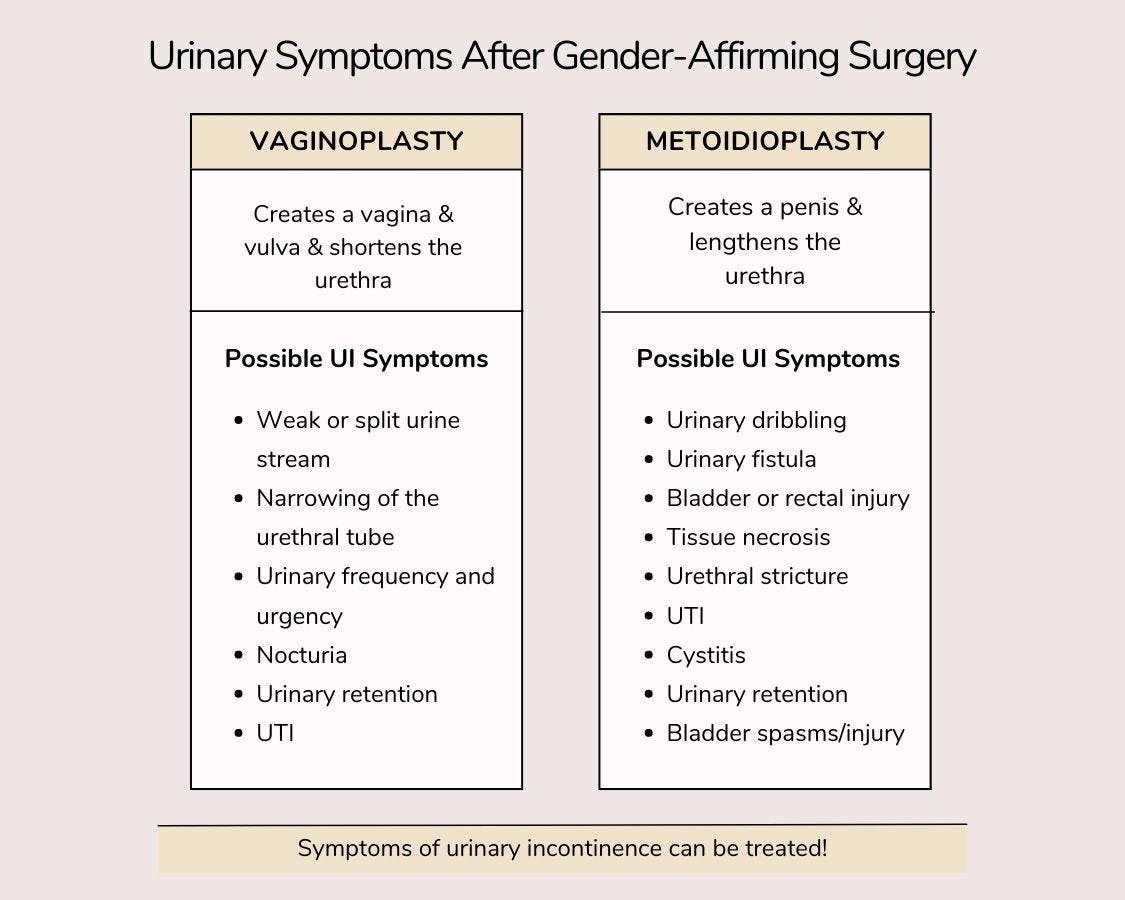
Both MTF and FTM procedures can result in UI. It’s highly common for urinary complications to arise after gender-affirming surgeries. Some of the most common procedures that cause UI symptoms are vaginoplasty and metoidioplasty.
Can Gender-Affirming Surgery Cause Urinary Incontinence?
When making the decision to undergo a gender-affirming surgical procedure, transgender women may elect to undergo a procedure that shortens their urethra, called a vaginoplasty. Other procedures include top surgery and thyrochondroplasty.
Vaginoplasty & UI Symptoms
Vaginoplasty creates female genitalia from the male organs which can shorten the urethra. In vaginoplasties, the prostate is relocated, which can cause challenges with urination and complete voiding. Because of this, some patients report the following symptoms:
- Weak or split urine flow.
- Narrowing of the urethral tube.
- Increase in urinary frequency and urgency.
- Nocturia (waking up at night to urinate).
- Urinary retention (the inability to empty the bladder), requiring catheterization.
- Urinary tract infection (UTI).
Metoidioplasty & UI Symptoms
After undergoing a FTM metoidioplasty, which lengthens the urethra and lengthens the clitoris, some patients report experiencing UI symptoms such as
- Urinary dribbling.
- Urinary fistula (irregular openings between organs in the urinary tract).
- Bladder or rectal injury.
- Tissue necrosis (death of tissues).
- Urethral stricture (closing or narrowing of the new urethra).
- UTI
- Cystitis
- Urinary retention.
- Bladder spasms or injury.
While these types of surgeries can cause urinary complications, they have been shown to increase the quality of life for transgender people. Following gender-affirming surgery, it’s reported that between 80% of people are satisfied with their sexual function, and 77% are satisfied with the aesthetic outcome of their procedures.
Treatments for Urinary Incontinence After Surgery
It can be difficult to feel that a surgery that’s supposed to help you feel more comfortable results in a challenge like UI. This is especially true for transgender individuals who undergo gender-confirmation surgery and develop UI because it can further impact their mental health when they are already at risk for mental health complications. One study showed that 32% to 50% of transgender people have attempted suicide, while another study showed 31% have major depressive disorder and 12% have general anxiety disorder.
It’s well known that UI can lead to mental health problems in many individuals due to the shame and embarrassment that’s attached to stigmas that surround the condition and its symptoms. Bladder problems like urine leakage can make people feel like they can’t live normally or that they need to miss out on certain activities to avoid accidents.
The good news is that UI is typically reversible or treatable with the right assistance from a healthcare provider or urology specialist!
Treatments for UI Symptoms
1. Toileting Techniques
You should discuss options for new toileting techniques post-surgery with your healthcare provider to find the best fit for your needs.


A stand-to-pee (STP) device can help align your preferred technique of toileting with your gender, but it can become complicated when using a male restroom that may have limited private stalls. Users of STP devices are also at risk for skin irritation and infections if the device is not cleaned diligently after each use.
Standing to urinate may also cause a hypertonicity of the pelvic floor muscles. This can lead to:
- Pain
- Dysfunctional voiding.
- Incontinence
- Constipation
However, a pelvic floor therapist can assist with these issues as they arise. And remember that sitting to urinate is okay, especially if it will improve voiding function and prevent discomfort.
2. Incontinence Products
Developing UI symptoms can make you feel as if you can’t enjoy all the activities you once did, but with the help of high-quality bladder control products, you can!
These discreet products are breathable and comfortable for daytime or nighttime wear. Their highly-absorbent cores soak up any leaks and keep you dry while maintaining skin health. Some products also come in male and female designs to look and feel like regular underwear. After undergoing gender-affirming surgery, we recommend the following products to protect yourself against leaks:
- Adult protective underwear: Protective underwear come in different designs for men and women. They’re thin, discreet underwear that have an elastic, pull-on waist and can be worn under your clothes.
- Bladder control pads: One of the most discreet options for individuals with incontinence, bladder pads are designed for the male and female anatomy. They can be worn inside your undergarments to protect against lighter leaks.
- Adult briefs: Adult briefs protect against heavier leakage and overnight incontinence. They have tear-away sides that make changing easy, which is an excellent choice for those recovering from surgery.


If you’ve been diagnosed with UI by a healthcare provider, you may qualify to get your bladder care products 100% free through insurance. See if you qualify!
3. Collagen Injections
This procedure consists of injecting collagen around the urethra and bladder neck to treat stress incontinence. There have been a small number of studies that show the advantages of periurethral collagen injections for people who experience UI after gender-affirming surgery; one study reported that both FTM and MFT individuals saw improvements in their UI symptoms after treatment.
4. Pelvic Floor Physical Therapy
Pelvic floor physical therapy (PFPT) can be beneficial if you’ve undergone gender-confirmation surgery. PFPT works by assessing your symptoms with a licensed pelvic floor physical therapist who specializes in the pelvic floor and pelvic floor disorders. After diagnosing your symptoms, your therapist will recommend certain treatments, such as:
- Biofeedback therapy.
- Pelvic floor exercises, such as kegel exercises (for men and women).
- Lifestyle modifications (diet, exercise, weight management, etc.).
5. Dietary Changes
Certain foods can irritate your bladder and cause irritation. It’s best to avoid these if you’ve had gender-affirming surgery and are experiencing UI symptoms to lessen leakage and urinary frequency. Foods to avoid include:
- Spicy foods.
- Tomato-based products.
- Caffeine, alcohol, carbonated drinks.
- Synthetic food dyes.
- Citrus fruits.
Knowing Your Healthcare Rights
It isn’t always easy to advocate for yourself, especially if you aren’t exactly sure what your rights are. We recognize that healthcare providers can (and do) break laws due to their own personal prejudices. However, we believe that it is important to know what your healthcare rights are, so you can properly defend and advocate for yourself if the situation arises.
Overall, there are federal and state laws that prohibit most public and private health insurance plans from discriminating against you simply because you are a transgender person. Healthcare providers cannot, under federal law, refuse to treat you or admit you because you are transgender. They cannot force you to have unnecessary examinations based on the fact that you are transgender. They also cannot refuse to treat you in accordance with your gender identity. This includes providing you access to restrooms that are consistent with your gender.
There are many ways that transgender people can advocate for themselves in making their lives more comfortable. One way we recommend is to ask your healthcare provider to provide a note that allows proper bathroom access at your workplace. This can ease anxiety and prevent the individual from waiting too long to void, causing additional urinary tract problems. While there are many other ways to advocate for yourself and your healthcare, we recommend visiting the below links for more information.
Since the topic of urinary incontinence after gender affirming surgery is relatively unexplored, it’s crucial to shed light on this issue and provide much-needed information, resources, and support for those who may be affected.
By openly discussing UI within the context of gender affirming surgery, we hope to empower individuals to seek appropriate care, reduce the stigma surrounding both gender-confirmation health services and UI, and form a sense of community among those navigating similar challenges.
It’s our goal to promote education, understanding, and compassion, and to contribute to a more inclusive and supportive environment for all who embark on the path of gender affirmation.
Healthcare Resources for Transgender Individuals
References
Cleveland Clinic. (2021, May 3). Gender Affirmation Surgery: What Happens, Risks & Benefits. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/21526-gender-affirmation-confirmation-or-sex-reassignment-surgery
NHS. (2017, October 23). Gender dysphoria. Nhs.uk. https://www.nhs.uk/conditions/gender-dysphoria/#:~:text=Gender%20dysphoria%20is%20a%20term
Meier, A. C., & Papadopulos, N. (2021). [Quality of life after gender reassignment surgery: an overview]. Handchirurgie, Mikrochirurgie, Plastische Chirurgie: Organ Der Deutschsprachigen Arbeitsgemeinschaft Fur Handchirurgie: Organ Der Deutschsprachigen Arbeitsgemeinschaft Fur Mikrochirurgie Der Peripheren Nerven Und Gefasse: Organ Der V..., 53(6), 556–563. https://doi.org/10.1055/a-1487-6415
The Impacts of SRS on Urinary Habits. (2022, March 22). ActivKare. https://activkare.com/blogs/news/the-impacts-of-srs-on-urinary-habits
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10073518/
Metoidioplasty Risks and Complications: Is Metoidioplasty Really Worth It? (n.d.). Metoidioplasty.net. Retrieved May 25, 2023, from https://www.metoidioplasty.net/risks-complications/
Hamidian Jahromi, A., Spellman, A. M., Horen, S., Cherullo, E. E., Dorafshar, A. H., & Schechter, L. S. (2022). A narrative review of outcomes following metoidioplasty: complications and satisfaction. Plastic and Aesthetic Research, 9(6), 41. https://doi.org/10.20517/2347-9264.2021.111
Nassiri, N., Maas, M., Basin, M., Cacciamani, G. E., & Doumanian, L. R. (2021). Urethral complications after gender reassignment surgery: a systematic review. International Journal of Impotence Research, 33(8), 793–800. https://doi.org/10.1038/s41443-020-0304-y
Virupaksha, H., Muralidhar, D., & Ramakrishna, J. (2016). Suicide and suicidal behavior among transgender persons. Indian Journal of Psychological Medicine, 38(6), 505. https://doi.org/10.4103/0253-7176.194908
Wanta, J. W., Niforatos, J. D., Durbak, E., Viguera, A., & Altinay, M. (2019). Mental Health Diagnoses Among Transgender Patients in the Clinical Setting: An All-Payer Electronic Health Record Study. Transgender Health, 4(1), 313–315. https://doi.org/10.1089/trgh.2019.0029
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.