Key Takeaways:
-
Your health insurance card is used to verify what's covered under your healthcare plan and informs you of what's covered under your benefits.
-
Insurance cards contain essential details like your policy number, prescription group number, and copay amounts, which you’ll need when getting health care.
-
Understanding the information on your insurance card helps you make informed decisions about your coverage and healthcare providers.
Your insurance card is an essential tool for navigating your healthcare coverage. It verifies your insurance status and ensures that you’ll be covered for medical services and healthcare provider visits.
Understanding the details on your card can help you get the most out of your benefits and connect with the right healthcare providers.
What Is a Health Insurance Member ID Card?
Health insurance member ID cards, also called insurance cards, are essential for verifying insurance coverage, confirming your insurance status, and ensuring accurate billing for medical services you receive. Insurance cards also allow healthcare providers to maintain current information about your insurance plan.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
How Can I Find the Coverage Details on My Health Insurance Card?
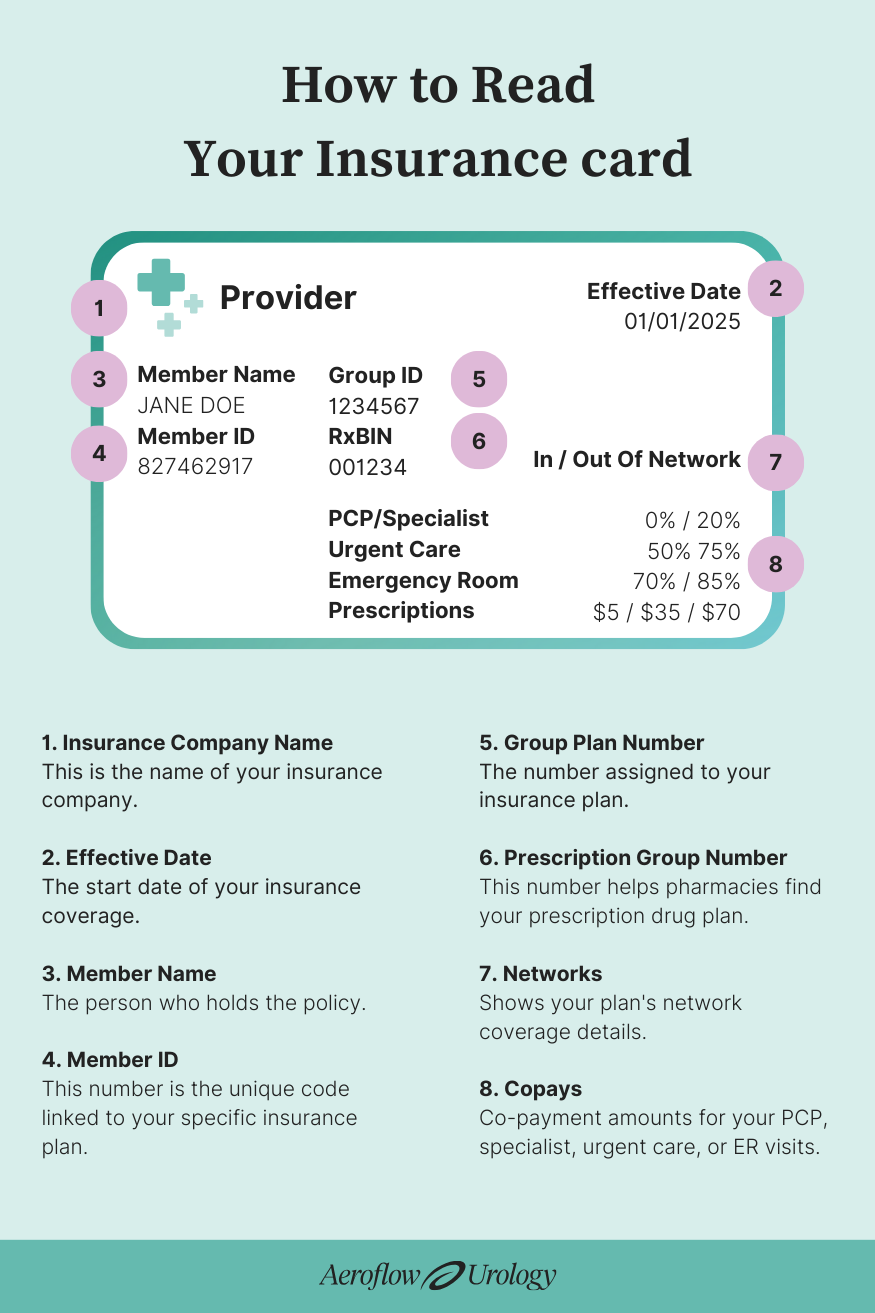
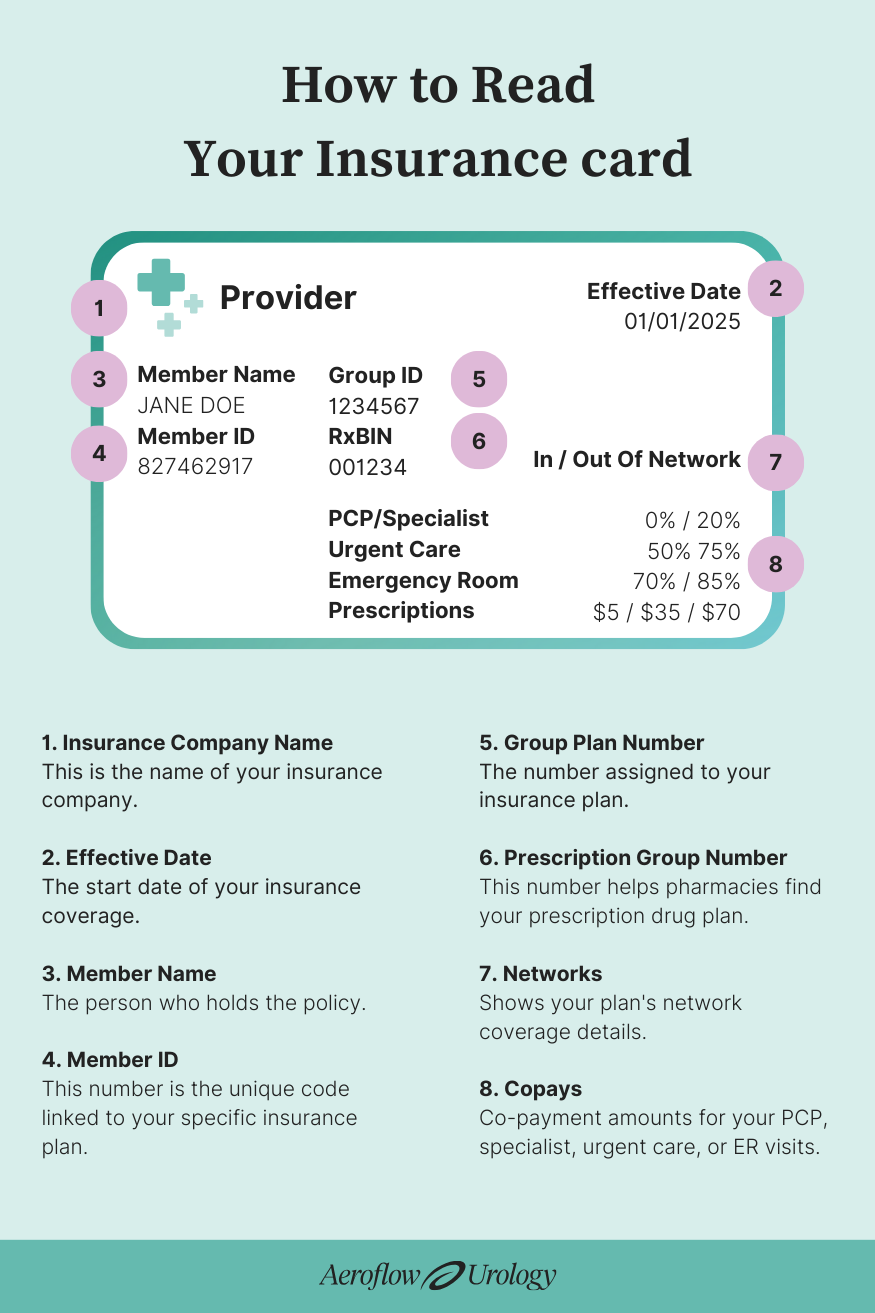
Once you’re enrolled in a health insurance plan, your card will be sent to the mailing address you provided when signing up for coverage. While all insurance card layouts vary by provider, your insurance information should be displayed on the front and back of your card.
Insurance Company Name
Your insurance company’s name and your type of plan should be listed at the top of the card. This is the name of your insurance company. Keep in mind that if you’re enrolled in a state Medicaid Managed Care Plan, it may be listed under a private company name, such as Blue Cross Blue Shield, Aetna, or UnitedHealth.
Insurance Company Contact Information
The back of your insurance card should display your insurance company’s contact information, including the company’s phone numbers, mailing address, and website. Use this information to call your insurance company phone number or visit their website to:
- Verify your coverage type and benefits.
- Find in-network healthcare providers and specialists.
- Confirm copays and other medical service costs.
Effective Date
Also called: Start date, date.
The effective date should be listed on the front of your insurance card and indicate the start date of your insurance coverage. Keep in mind that not all insurance cards have effective dates on them.
Member Name
Also called: Subscriber name, policyholder name, members.
The policyholder’s name (whether it’s yours or a loved one’s) should be displayed on the front of the insurance card. If you are the policyholder and have family members on your insurance plan, their names will be listed in this area.
It’s important to remember that if you’re using your insurance card to apply for free incontinence supplies, you should submit your name exactly as it appears on your insurance card.
Member ID
Also called: Subscriber ID, policy number, policy ID.
Your policy number, sometimes called your subscriber ID or member ID, should be listed on the front of the card. These three terms can be used in place of one another. This number is the unique code linked to your specific insurance plan.
Group Plan Number
Also called: Insurance group number.
A group plan number, also called an insurance group number, should be listed on the front of your insurance card if you receive insurance coverage through your employer. This number is assigned to your insurance plan.
Keep in mind that not all insurance cards will have a group plan number.
Prescription Group Number
Also called: Prescription ID, prescription number, RxBIN.
Your prescription group number may be displayed on the front of your card. The prescription group number is a unique identifier that helps pharmacy providers determine the specific prescription drug plan your insurance offers.
Networks
Also called: In-network, out-of-network.
The front of your insurance card may list your network percentages. The in-network provider percentage shows how much your insurance company pays healthcare providers who are in their provider network. The out-of-network provider percentage shows how much your insurance company pays healthcare providers who are outside of their provider network. With out-of-network providers, you typically have to pay the cost that your insurance does not cover.
Copays
Also called: Co-payment, PCP copay, emergency room copay, specialist copay.
Copay types and amounts should be listed on the front of your insurance card. These amounts refer to how much your co-payment will be when you visit your primary care provider (PCP), a specialist, urgent care, or an emergency room.
Insurance Card FAQs
When will I get my insurance card?
You should receive your insurance card through the mail at the address you listed when signing up for coverage after you’ve been enrolled in a health insurance plan.
Is my policy number the same as my member ID number?
Your policy number is the same as your member ID number. These terms are used interchangeably depending on the type of card you have.
What if I can’t find certain insurance information on my card?
If you have trouble finding any information about your insurance coverage plan, call the number for members listed on the back of the card.
How often do I get a new member ID card?
You’ll typically receive a new insurance card when your insurance plan changes. Examples include changes made during open enrollment or after you’ve changed personal information. In general, insurance companies issue new cards annually, but you may receive a new one at any time if there are adjustments to your benefits, a change in your insurance provider, or a switch in your coverage level.
What do I do if I lose my insurance card?
If you lose your card or need a replacement, you can request a new one from your insurance company.
Why does Aeroflow Urology need my insurance information to check my coverage for free incontinence products?
To verify your eligibility for free incontinence products, we need your insurance details, state information, and some personal information. This is because qualification guidelines vary by state and insurance plan. Additionally, your coverage may depend on your unique needs or medical condition.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.