Key Takeaways:
- Children with autism commonly experience loss of bladder or bowel control, known as incontinence.
- By being supportive, using incontinence products, and speaking with your child’s pediatrician, you can help your child overcome their symptoms.
- Your child may qualify to receive free incontinence products with Aeroflow Urology.
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Each and every child will encounter challenges as they grow older, whether that's learning to speak, potty training, or even learning to walk. However, children with an autism diagnosis can sometimes have even more unique sets of challenges. Specifically, one of those unique challenges may be incontinence.
Typically, children with autism spectrum disorder (ASD) will grow out of their incontinence as they grow older. Sometimes, however, it may take longer to establish effective toilet training practices.
Autism, with the addition of incontinence, may seem overwhelming at first, but there are proven ways to manage incontinence in both younger and older children with autism without having to make drastic changes to your daily routine.
What Is Incontinence?
Incontinence is defined as the lack of voluntary control of urination or defecation. There are many different types of incontinence; Urinary incontinence is the loss of bladder control, and fecal incontinence is the loss of bowel control.
Incontinence is often prevalent in children with autism and other disabilities due to common delays in potty training. Some nonverbal children with autism may also not be able to communicate the need to use the restroom, resulting in unwanted accidents.
We recognize that children with autism have unique, special needs that are specific to each child. Essentially, there is no one clear answer. It can take some trial and error before you establish what is best for your child and their unique needs.
In some cases, children with autism may experience urge incontinence, where they don’t realize the need to urinate until they feel a sudden, unexpected urge, and the bladder contracts when it shouldn’t. Children can also become distracted by video games or other stimulating activities, in which they may not recognize the urge to urinate.
In other cases, incontinence can only be managed, but incontinence treatment can help some children successfully use the restroom on their own without the need for youth diapers or training pants (pull-ups).
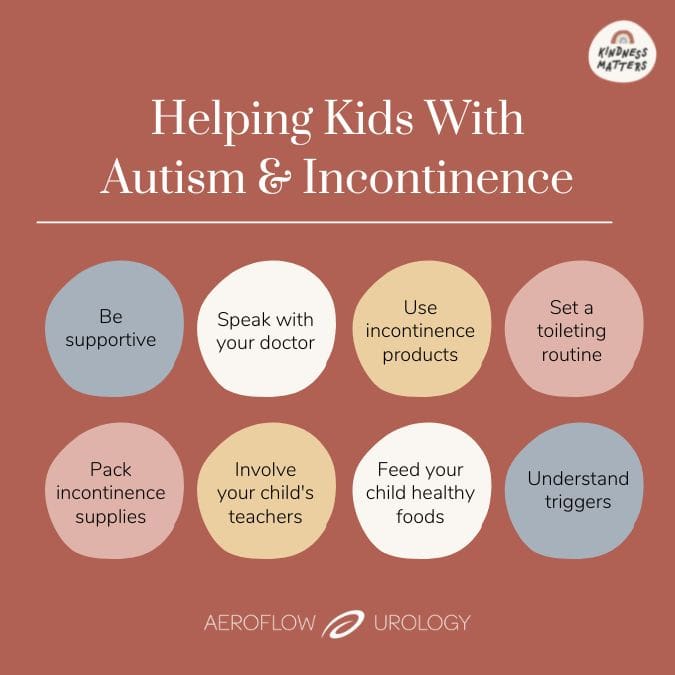
8 Ways to Help Your Child With Autism & Incontinence
There are many ways you can help support your child while they manage their incontinence. Read our top 8 tips from Samantha Eaker DNP, CPNP-PC, to set your child up for success.
1. Be Supportive
The first key to success in helping your child manage their incontinence is to be supportive and understanding.
This may be a given, but it is important to assure your child that incontinence does not have to be a bad thing or something that lasts forever. You may need a lot of patience and persistence to help your child manage (or overcome) their incontinence, but there are ways to make it easier on both you and your child.
2. Speak With Your Healthcare Provider
If your child starts to experience incontinence or symptoms of the condition, such as delayed toilet training, nocturnal enuresis, or bladder leakage, it is important to seek help from a healthcare provider.
A trip to your child's pediatrician will allow you to decipher if the incontinence symptoms are due to the effects of your child's autism or another underlying medical diagnosis. Other medical diagnoses will have varying treatment plans, but if your child is clear of any other medical diagnosis that could be causing the symptoms, their incontinence treatment will involve a more hands-on approach.
3. Use Incontinence Products
Symptoms of autism can include resistance to change, so it may take a little extra work with your child to take steps towards using diapers or pull-ups less. As your child's primary caregiver, remember that you know them best.
When trying a new method of toilet training, or removal of diapers, we recommend taking 2 weeks to ensure that your child has enough time to truly adjust to the changes. Using interval continence care products such as training pants or pull-ups can also be beneficial in the training process from diapers to regular underwear.
Also, if your child exhibits signs of an incontinence schedule, such as only passing stool in their pull-up after they eat lunch, you may have an opportunity to anticipate the incontinence event and intervene.
4. Set & Stick to a Toileting Routine
Another method of helping your child manage their incontinence symptoms is to keep track of your child’s normal bathroom routine.
Knowing roughly when and how often your child uses the restroom will enable you to be able to remind them that it may be time to use the restroom before an accident occurs. It can be good practice to have your child use the restroom every 2-3 hours, depending on the usual schedule. A Bladder Diary can be a great tool to track accidents, as well as other contributing factors.
If your child doesn’t want to stop engaging in an activity for a bathroom break, pause and remind them that it will still be there when they get back. We recognize that this can potentially cause meltdowns to occur, but it is important to try different methods of working with your child to ensure their success.
5. Carry Incontinence Supplies With You
It is also beneficial to plan ahead and always be prepared for activities outside of the home.
This can be achieved by ensuring your child has enough incontinence products to last through the event.
Keeping a bag with extra pull-ups and a change of clothes can be a great way to combat potential incontinence episodes. Underpads (or chux) can also help mattresses stay clean and dry during your child's sleepovers.
6. Involve Your Child's Teachers
It can be very beneficial to inform your child’s teachers about their incontinence so they can set your child up for success by:
- Allowing your child to sit close to the restroom.
- Allowing your child to go to the restroom without permission.
- Developing a private codeword for accidents.
- Assisting with changing and clean-ups if accidents happen.
- Ensuring that extra pull-ups or other incontinence products are readily available if needed.
7. Understand Your Child's Specific Triggers
When potty training, children with autism can encounter sensory triggers in the restroom.
Whether the flushing of the toilet is too loud or the toilet seat is uncomfortable, it is important to be aware of what might be discouraging your child from using the restroom.
Flushing the toilet once they leave the bathroom and special toilet seats are good ways to help your child with these sensory triggers.
8. Feed Your Child Healthy Foods
Another way to set your child up for success is by equipping them with a healthy diet with plenty of fluids.
Oftentimes, young children don’t drink enough water which can contribute to constipation and worsened incontinence symptoms. Constipation can cause bloating of the abdomen, which can then lead to increased pressure on the bladder. Fruits and vegetables that are rich in fiber may help with battling constipation, as well.
It is important to contact your doctor if your child’s stomach is swollen, if the stomach is in prolonged pain that doesn't react to medication, or if your child goes an entire week without a bowel movement.
Q & A With Daily Autism Family
Marc and Melissa, from the Daily Autism Podcast, have a son with autism named Cal. Aeroflow Urology partnered with them and asked Melissa a few questions about how they have managed Cal’s autism and incontinence.
Read her responses below or watch the extended video in this article!
Q: How did you approach toilet training with Cal?
A: Our potty training journey began when Cal was 2 1/2 years old. We started by introducing different videos and books, and picking different potty seats to see what fit him the best— we actually ended up using the regular toilet. And then, we had him pick his underwear so he could get excited, so he picked baby shark.
Q: How did you determine when Cal was ready for toilet training?
A: I realized at 3 years old, after we had started trying with his therapist, that we needed to give it more time. So there were times when we took breaks and then came back to it, and there were times when we tried more than others. He potty trained with all his therapists, but I realized that developmentally, he just wasn’t ready yet. He didn’t care that he was wet, and he had really no signs that he was ready to potty train.
Q: What is your potty training routine like?
A: A good routine we established with us and his therapist is we’d have him get undressed, go on the potty before he got in the shower or bath. He’s very good about going to the potty then, but one thing with Cal— being diagnosed with autism— he is very rigid.
He has cognitive rigidity, which means he will go for his therapist, but he won’t go for me. He picks very specific people to do very specific things for him, and me with potty training? He does not want to do— except for going to the bathroom before he goes in the shower.
It’s just something you can’t push with him. I have to realize, eventually, he’s going to be okay going for me, it’s just getting over that strict rigidness that he has.
Q: What advice do you have for other caregivers or parents when it comes to encouraging children with autism to potty train?
A: Keep trying! I do think incentives are great; if your kid likes books, stuffed animals, puffy stickers, candy— it’s positive reinforcement, and I think it’s a good thing because they should be rewarded because they’re trying just as hard as you are. Don’t give up, definitely keep trying. It is going to take time. Everybody learns differently and grasps things at different times, so give yourself time, give yourself grace, and it will happen.
How to Get Free Incontinence Supplies Through Medicaid
Managing incontinence can be overwhelming at times. However, Aeroflow Urology can assist in supplying incontinence supplies through your Medicaid and other Medicaid-managed care plans.
Not only will this service be beneficial financially, but it can also alleviate stressful store trips. Instead of running out to the store for youth diapers and pull-ups last minute, fill out our secure Eligibility Form to get started.
If approved, your child's incontinence supplies will be shipped directly to your home in discreet packaging on a monthly basis - ensuring privacy and ease of use.
One of our Continence Care Specialists will be matched with your child to ensure they have correctly fitting products. Our Specialists will also check in on a monthly basis to see if any changes need to be made, such as switching sizes as your child grows, or switching to a product with more or less absorbency.
Jump To: Top | Eligibility Form
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.