Key Takeaways:
- Anorexia nervosa and bulimia nervosa can negatively impact bladder and pelvic floor health.
- Malnutrition, constipation, muscle wastage, vomiting, and other factors of eating disorders can contribute to symptoms of urinary incontinence.
- At-home and in-office treatments can help reduce symptoms of incontinence and help manage eating disorders.
An eating disorder is a mental illness that encompasses a spectrum of behaviors and side effects that take a toll on individuals experiencing the condition. Eating disorders can make people feel shameful, depressed, and isolated, and many experience heart, hormonal, and digestive problems.
In addition to the widely-known effects this condition can have on individuals’ bodies and minds, eating disorders can also harm the urinary system. It’s essential to understand the connection between eating disorders and urinary incontinence to prevent and treat symptoms so you can live healthily.
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Types of Eating Disorders
Eating disorders (EDs) affect a large swath of the population; it’s estimated that 28.8 million Americans will experience it in their lifetimes. While some would typically correlate females with EDs, it’s been shown that males account for 25% of people with the condition. EDs can have many side effects, and 10% even result in death.
Types of eating disorders include:
- Anorexia nervosa: Characterized by food restriction that leads to low body weight. Anorexia is commonly associated with a distorted body image.
- Bulimia nervosa: Also called binge-eating disorder, this is characterized by the consumption of large quantities of food in a short period, followed by self-induced vomiting (purging), strict dieting, or extreme exercise.
Can Eating Disorders Cause Bladder Problems?
Eating disorders can cause bladder problems, known as urinary incontinence (UI). UI is defined as the loss of bladder control, often leading to urinary leakage.
Types of Incontinence Caused by Eating Disorders
- Urge incontinence / overactive bladder (OAB): Feeling a sudden and intense urge to urinate, urinating more frequently than usual, and leaking urine. This type of UI is prevalent among people with EDs.
- Overflow incontinence: Dribbling or leaking urine throughout the day after voiding the bladder due to the inability to empty the bladder completely.
- Stress incontinence: Leaking urine when coughing, sneezing, vomiting, bending over, or exercising due to weakened pelvic floor muscles and pressure on the bladder.
- Functional incontinence: Leaking urine due to the inability to make it to the restroom on time.
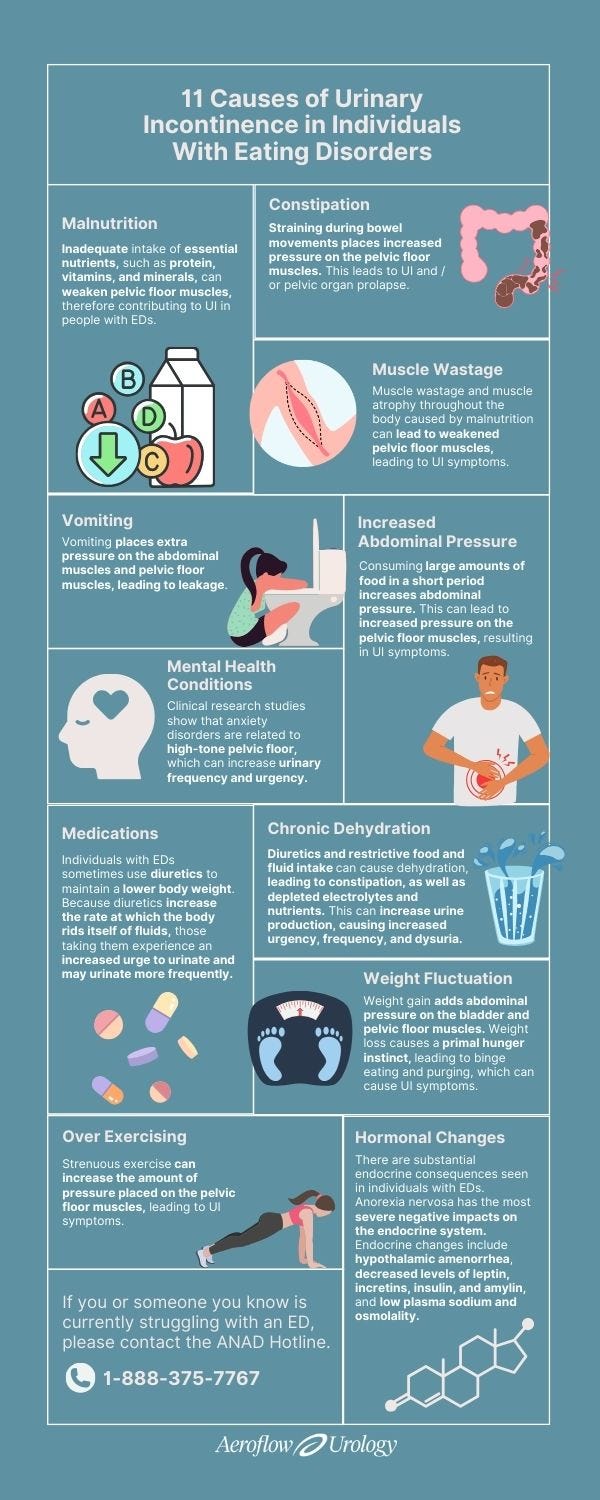
11 Causes of Urinary Incontinence in Individuals With Eating Disorders
While anorexia nervosa seems to cause a slightly greater risk of UI symptoms, the following factors contribute to the increased risk of all urinary symptoms due to the side effects of bulimia and / or anorexia.
1. Malnutrition
Inadequate intake of essential nutrients, particularly those that support muscle and connective tissue health, such as protein, vitamins, and minerals, can weaken pelvic floor muscles, contributing to UI in people with EDs.
Malnutrition also leads to functional hypothalamic amenorrhea, diminishing hormone levels in the genitourinary tissues. These changes are similar to the changes seen in genitourinary syndrome of menopause. This causes increased urinary urgency, frequency, and even increased risk of urinary tract infections (UTIs).


2. Chronic Constipation
Constipation is common among those with EDs. Constipation leads to straining during bowel movements and places increased pressure on the pelvic floor. This leads to UI and / or pelvic organ prolapse.
Constipation and the muscle tension seen with the anxiety experienced by those with EDs can cause dysfunctional nerve functioning in the pelvis, either causing overactive or decreased nerve sensation. The decrease in nerve sensation can cause neurogenic bladder and overflow incontinence.
The large amounts of food consumed by individuals with bulimia can also cause abdominal pain and bloating, leading to constipation, which has a direct correlation with UI symptoms.
3. Muscle Wastage
Muscle wastage and muscle atrophy throughout the body caused by malnutrition can weaken pelvic floor muscles, leading to UI symptoms.
4. Vomiting
Vomiting, which is often seen in individuals with bulimia, places extra pressure on the abdominal and pelvic floor muscles, causing stress incontinence.
5. Increased Abdominal Pressure
When those with binge-eating disorders consume large amounts of food in a short period, abdominal pressure increases. This can lead to increased pressure on the pelvic floor muscles, resulting in UI symptoms.
6. Mental Health Conditions
Studies show that mental disorders, such as stress, anxiety, and trauma, increase an individual’s risk of developing UI. Clinical research studies also support anxiety disorders related to hypertonic pelvic floor, leading to increased urinary frequency and urgency.
These mental health conditions— especially anxiety disorders— are often seen in people with EDs. There is also a strong correlation between UI and underlying personal traits of perfectionism and the need for control seen in individuals with EDs.
Those with EDs are typically in a sympathetic nervous system state. This “fight-or-flight” setting tenses the muscles, increasing the need to void more frequently and incomplete bladder emptying.
The survival protectiveness seen in individuals with EDs often leads to muscle tension that is not as readily available for movement and support, causing instability in the pelvic girdle. This results in UI, abdominal / pelvic pain, constipation, bloating, and catastrophizing thoughts that continue to contribute to the cycle of tension and UI.
7. Medications
Individuals with EDs sometimes use diuretics to maintain a lower body weight. Because diuretics increase the rate at which the body rids itself of fluids, those taking them experience an increased urge to urinate and may urinate more frequently.
The abuse of laxatives is also commonly seen in people with EDs. Taking laxatives frequently may lead to the inability to have a bowel movement, resulting in constipation and UI symptoms.
Some people with EDs may also be prescribed antidepressants, which can affect bladder control.
8. Chronic Dehydration
Diuretics and restrictive food and fluid intake can cause dehydration, leading to constipation, electrolyte imbalances, and nutrient imbalances. This can increase urine production, causing increased urgency, frequency, and dysuria.
Chronic dehydration also concentrates the urine, leading to irritation along the lower urinary tract, causing increased urgency, frequency, leakage, and increased risk of UTIs.
9. Weight Fluctuation
In many individuals with EDs, weight fluctuates. Weight gain can add abdominal pressure on the bladder and pelvic floor muscles. Weight loss can cause a primal hunger instinct, leading to binge eating and purging, which can cause UI symptoms.
10. Hormonal Changes
There are substantial endocrine consequences seen in individuals with EDs. Anorexia nervosa has the most severe negative impacts on the endocrine system. Endocrine changes include:
- Hypothalamic amenorrhea: Long periods of amenorrhea can lead to infertility, bone loss, increased risk of dementia / Alzheimer’s disease, hair loss, and fatigue.
- Decreased levels of leptin, incretins, insulin, and amylin: Can cause harmful effects on bone and neurocognition, leading to depression, anxiety, and eating disorder psychopathology.
- Low plasma sodium and osmolality: Those with anorexia have lower plasma sodium and osmolality levels, along with higher levels of antidiuretic hormone, which can lead to concentrated urine, irritation to the lining of the bladder, dysuria, UTIs, and UI.
11. Excessive Exercise
Many individuals with EDs compulsively exercise, commonly referred to as “problematic use of physical activity.” Strenuous exercise can place extra pressure on the pelvic floor muscles, leading to UI symptoms. In fact, female athletes with EDs have been found to be 3 times more likely to have UI symptoms than those without the condition.
Treating Eating Disorders & Bladder Problems
If you’re currently struggling with an ED, call the Anorexia Nervosa & Associated Disorders (ANAD) hotline at 1-888-375-7767.
- Get proper exercise. It is essential to find the balance between building strong muscles and exercising for thinness. Working with a personal trainer or physical therapist with expert knowledge of eating disorders is key in helping you optimize movement to support your body. Proper exercise may also decrease symptoms of UI.
- Speak with your healthcare provider. Embarrassment around UI is very common, and it may be even more difficult for you to speak with your provider openly about UI symptoms if you are managing an ED. However, it’s critical that you talk with a doctor to treat your ED and UI symptoms. Your healthcare provider can help balance your hormones, improve nutrition, and alleviate UI. In many cases, it is reversible!
- Work with a mental health professional. Many individuals with EDs face mental health challenges, and conditions like anxiety, stress, and trauma can be the leading causes of EDs. Speak with a mental health professional, such as a therapist or psychologist specializing in EDs.
- Work with a nutritionist. Ask your primary physician for a referral to a nutritionist who has experience or training in eating disorder treatment. Your nutritionist can help optimize your food intake to fuel, support, and heal your body, eventually reducing UI symptoms. Finding nutritional balance is the foundation for improving UI and is needed before undertaking behavioral changes to improve symptoms.
- Eat a healthy, complete diet. It’s a good idea to increase your intake of:
-
- Healthy fats (olive oil, avocado, etc.).
- Protein
- Fiber
- Water


Avoiding foods that irritate the bladder and bowels is also essential! Avoid alcohol, spicy foods, caffeine, and tomato-based products.
- Go slowly. It’s important that if you’re making any changes to your habits or diet— either at home or with a healthcare professional— you go slowly to help avoid psychological control or binge eating behaviors.
- See a pelvic floor physical therapist (PFPT). Pelvic floor physical therapy is a highly specialized and trained form of medical therapy that focuses on improving the function of the pelvic floor muscles. Seeing a PFPT may help reverse and treat symptoms of UI.
- Do pelvic floor exercises at home. Pelvic floor exercises, such as Kegels, can be done in the comfort of your home to reverse UI symptoms. These exercises have been proven to help UI.
- Avoid OAB medications. OAB medications are not helpful in these situations and may increase the risk of constipation. Speak with your healthcare provider about using alternative methods to relieve UI symptoms.
- Use incontinence products. Incontinence products, such as adult pull-ons and bladder control pads, will keep you comfortable and dry as you manage your UI. If you’ve been diagnosed with incontinence by a healthcare professional, you may be able to get your products for free through insurance with Aeroflow Urology! See if you qualify in under 5 minutes today with our simple, secure Eligibility Form.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
It can take quite a bit of time to work on lifestyle and behavioral changes needed to heal from EDs. However, by working with healthcare professionals and speaking with them openly about your UI and ED symptoms, it is possible.
Jump To: Top | Eligibility Form
References
Eating Disorder Statistics | ANAD - National Association of Anorexia Nervosa and Associated Disorders. (2023, November 29). Anad.org. https://anad.org/eating-disorder-statistic/
Debus, G., & Kästner, R. (2015). Psychosomatic Aspects of Urinary Incontinence in Women. Geburtshilfe Und Frauenheilkunde, 75(02), 165–169. https://doi.org/10.1055/s-0034-1396257
Copeland, P. M. (1989). Diuretic Abuse and Central Pontine Myelinolysis. Psychotherapy and Psychosomatics, 52(1-3), 101–105. https://doi.org/10.1159/000288307
Ng, Q. X., Lim, Y. L., Loke, W., Chee, K. T., & Lim, D. Y. (2022). Females with Eating Disorders and Urinary Incontinence: A Psychoanalytic Perspective. International Journal of Environmental Research and Public Health, 19(8), 4874. https://doi.org/10.3390/ijerph19084874
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.