Key Takeaways:
- Rheumatoid arthritis is a chronic autoimmune disorder that causes joint inflammation.
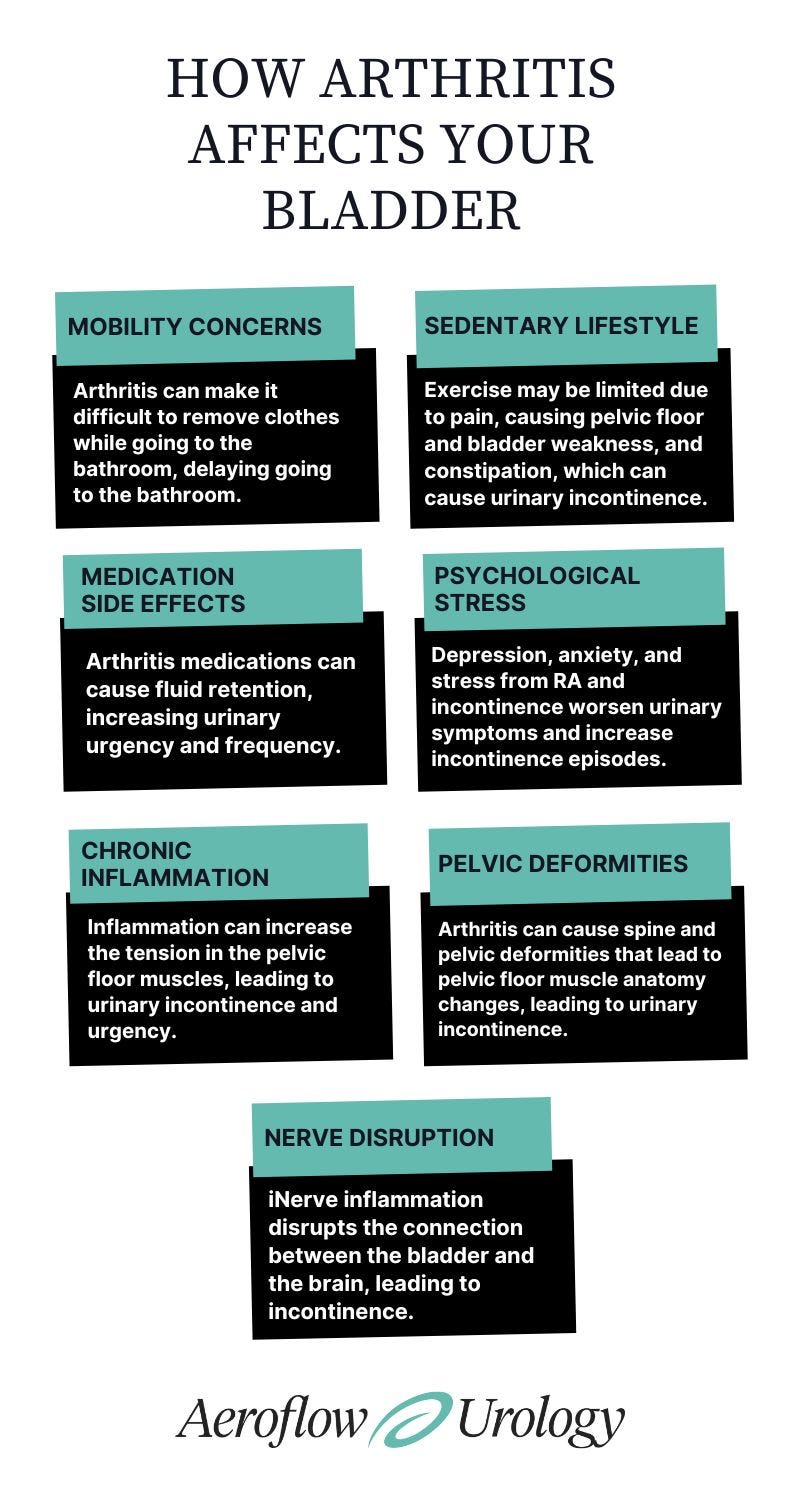
- Mobility concerns, a sedentary lifestyle, medication side effects, nerve disruption, and more can lead to urinary incontinence in those with rheumatoid arthritis.
- Treatments may include using free bladder control supplies, an anti-inflammatory diet, and pelvic floor physical therapy.
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Rheumatoid arthritis is not just a condition affecting the joints; it can impact various aspects of health, including the urinary system.
From medication side effects to nerve disruption, if you have arthritis, you may experience urinary incontinence, posing additional challenges to your daily life.
Let's explore the connection between rheumatoid arthritis and urinary issues and discuss practical strategies for managing both conditions.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease that can cause damage to the body in which your immune system attacks its own tissues.
RA damages different parts of the body, such as nerve tissues, eyes, and heart. Hands and wrists are commonly affected joints, and these areas can become swollen and painful.
Specific types of arthritis include rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and osteoarthritis. Gout and systemic lupus erythematosus are not always considered arthritis-related; however, the inflammation from both types of arthritis can significantly impact the bladder.
The cause of RA is unknown, but it may be caused by genetics.
Symptoms of RA
- Swollen joints.
- Warmness in the joints.
- Joint stiffness.
- Joint pain.
- Fever
- Loss of appetite.
- Fatigue
How Does Rheumatoid Arthritis Cause Bladder Problems?
RA can lead to a variety of bladder and bowel problems, also known as incontinence. The most common type of incontinence experienced by individuals with RA is called urge incontinence.
Urge incontinence occurs when you feel a sudden and uncontrollable urge to urinate, resulting in leakage.


Mobility Concerns
Arthritis in the hands and wrists can make it difficult to remove your clothes while going to the bathroom, which may lead to accidents. Lower extremity arthritis can decrease mobility, causing a delay in making it to the restroom in time to void. This is known as functional incontinence.
Sedentary Lifestyle
With RA, you may limit exercise or physical activity because you're in pain. While this helps to decrease the pain, a sedentary lifestyle can cause pelvic floor and bladder weakness, along with constipation, which, in turn, can also cause urinary incontinence.
Medication Side Effects
Some arthritis medications can cause fluid retention, increasing urinary urgency and frequency.
- NSAIDs. These medications do not directly impact urinary incontinence. However, these increase the risk of fluid retention and increase urinary incontinence, including frequency and urgency, especially with long-term NSAID use.
- Corticosteroids. Cause fluid retention, electrolyte imbalances, and increased urinary volume output. This increase in volume can increase urinary frequency and urgency.
- Disease-modifying antirheumatic drugs (DMARDs). These types of medications help to control inflammation. While they don't directly impact the bladder, some individuals have noted increased urinary incontinence upon starting them.
- Biologics. For more severe cases of arthritis, you may need a medication that falls within this class of drugs. Biologics decrease the immune system and can lead to urinary tract infections (UTIs), which lead to urinary urgency and incontinence.
- Opioids. While occasionally prescribed for arthritis pain, healthcare providers try to avoid these as much as possible. Should these medications need to be prescribed, opioids may cause constipation that leads to urinary incontinence.
Psychological Stress
The mental health connection is also significant; if you're living with chronic pain, like the type you may experience with RA, you may experience depression, anxiety, and stress. These psychological factors can worsen urinary symptoms and increase incontinence episodes.
Chronic Inflammation
Chronic inflammation affects the bladder by causing increased fluid retention and possible kidney damage. Inflammation can increase the tension in the pelvic floor muscles, leading to urinary incontinence and urgency.
Long-term inflammation can cause damage to the joints and bones, leading to changes in posture and alignment of the spine and pelvis, which can cause added abdominal pressure on the pelvic organs, including the bladder. This will lead to increased urgency and incontinence.


Pelvic Deformities
Arthritis can cause spine and pelvic deformities that lead to pelvic floor muscle anatomy changes. These shifts in the pelvic floor muscles cause dysfunctional movements and poor coordination, leading to urinary incontinence, urgency, and frequency.
Nerve Disruption
Inflammation from arthritis mainly affects the joints. This inflammation can extend to nearby tissues, like nerves, damaging the nerve directly and disrupting nerve signaling. This disruption can impact the connection between the bladder and the brain, leading to incontinence.
Some joint deformities can cause nerve compression and disrupt signaling. Autoimmune arthritis may also attack the nerves, causing a signal interruption.
Treating Rheumatoid Arthritis & Incontinence
Thankfully, there are many ways to manage RA and incontinence.
- Free bladder control supplies. If you're experiencing urinary incontinence due to RA, you may be able to receive free protective supplies from Aeroflow Urology {Link to uro block at bottom}. We work with Medicaid managed-care plans to get people the free bladder control supplies they need to improve their quality of life and manage leaks confidently.
- Pelvic floor physical therapy. Pelvic floor physical therapy can assist with your limitations and specific mobility concerns. Your therapist will focus on the areas of concern and pain and look at muscle coordination around the pelvic floor muscles. The sooner physical therapy can be integrated, the more you may delay progression and improve your symptoms. Benefits of pelvic floor therapy include increased mobility, improved bladder function and control, improved defecation with less straining, and decreased pain.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
3. Anti-inflammatory diet. An anti-inflammatory diet can help decrease systemic inflammation. Increased water intake and fiber intake are other great ways to improve overall health. Nutrition—especially increased protein, vegetables, fruit, and whole grains—will help support the muscles and improve stability. Probiotics have also been shown to support the gut microbiome and improve pain through decreasing inflammation.
4. Mental health support. Working with a mental health provider can significantly improve acceptance and growth of your conditions. Mindfulness and meditation have also been shown through multiple studies to improve pain and acceptance.
5. Open communication. One of the biggest challenges with these conditions is the silence around arthritis and urinary incontinence. Most healthcare providers do not bring up the conversation, and then you feel that it is not important. Be open with your provider and let them know about your symptoms so you can create a treatment plan.
6. Physical movement. The more the body moves, the more the muscles can work efficiently. Pelvic floor exercises and core exercises will help with stabilization and bladder function. Again, working with a pelvic floor therapist can be helpful in individualizing your exercise routine based on your needs. Walking and aquatic exercises have been shown to improve mobility and decrease pain greatly.
7. Low-intensity shockwave therapy. Low-intensity shockwave therapy has been shown to decrease inflammation and improve pain. This technology can improve urinary symptoms by reducing inflammation and pelvic floor tension.
8. Daily lifestyle modifications. Avoid constipation, increase your fluid intake, get enough fiber, decrease bladder irritants (caffeine, alcohol, spicy foods, tomato-based products, etc.), and get optimal sleep.
9. Outside resources. The National Continence Society, Aeroflow Urology, and the Arthritis Foundation have resources you can use if you're managing RA and incontinence. The Aeroflow Urology Adult Facebook Group is also a safe place where you can find support and have honest discussions about managing incontinence.
Managing RA and incontinence may seem impossible at times, but by communicating with your healthcare provider, finding support, and making small lifestyle adjustments, there is hope to improve incontinence symptoms.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.