Key Takeaways:
- Male pelvic floor muscles control the bladder and bowels, provide organ support, and contribute to stability and sexual function.
- Men can seek professional help, do pelvic floor exercises, like Kegels, and explore other treatments to care for their pelvic floors.
Too often, men forget about the health of the pelvic floor. Still, it is vital in everyday physiological functions, such as controlling your bowel and bladder continence and sexual function.
If you ignore this group of muscles, you may end up with a weak pelvic floor, leading to incontinence.
Read this post to learn why you should care about your pelvic floor and how to improve pelvic floor health.
Jump To:
What Are the Male Pelvic Floor Muscles?
Why Is the Male Pelvic Floor Important?
What Causes Pelvic Floor Dysfunction & Incontinence in Males?
What Are the Symptoms of Pelvic Floor Dysfunction in Males?
How Can Males Strengthen Their Pelvic Floor Muscles?
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
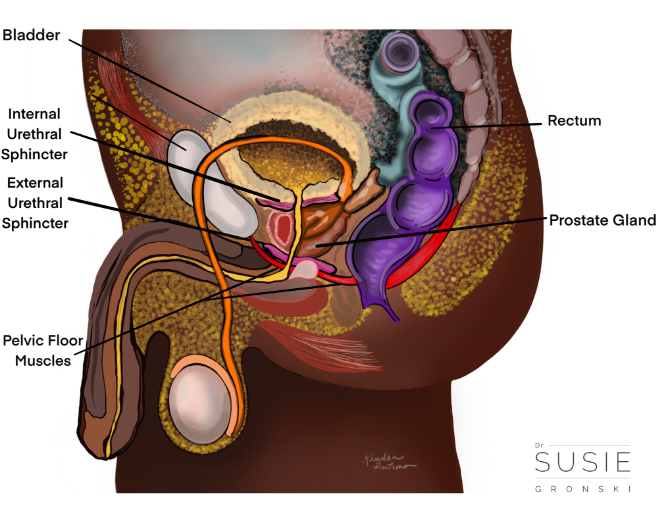
What Are the Male Pelvic Floor Muscles?
You should think of the pelvis like a large bowl of cereal. The pelvic floor muscles make up the bottom of the bowl, and the pelvic organs rest inside like cheerios floating around in your breakfast bowl.
To find your pelvic floor muscles while sitting, you can slide your hands under your sitz bones (the bony parts of the butt that you're sitting on). Your pelvic muscles are located between those sitz bones, extending from your pubic bone (at the front) to your tailbone (at the back).
The pelvic floor supports the following structures:
- Bladder
- Rectum
- Prostate
- Erectile tissues.
- Digestive organs.
3 Muscle Groups of the Male Pelvic Floor
Three muscle groups make up the pelvic floor.
- The outermost layer of muscles helps with orgasm, ejaculation, urination (allowing the urethra and bladder to empty), and bowel control.
- The middle layer is a group of muscles that add another layer of support around the urethra to prevent peeing during exertion, strengthen fascial connections with your urogenital structures, and help stabilize the pelvis and lower spine during movement.
- The innermost layer of the pelvic floor is a group of muscles called the levator ani, which means to "lift the anus." This group of muscles is commonly known as the pelvic diaphragm. These muscles support the pelvic organs (bladder, prostate, and rectum) nestled in the pelvic bowl. This group of muscles also helps you poop. These tiny little muscles are marathon runners; Their endurance and function are necessary to help reinforce the structural integrity of the pelvis provided by ligaments and connective tissue.
Why Is the Male Pelvic Floor Important?
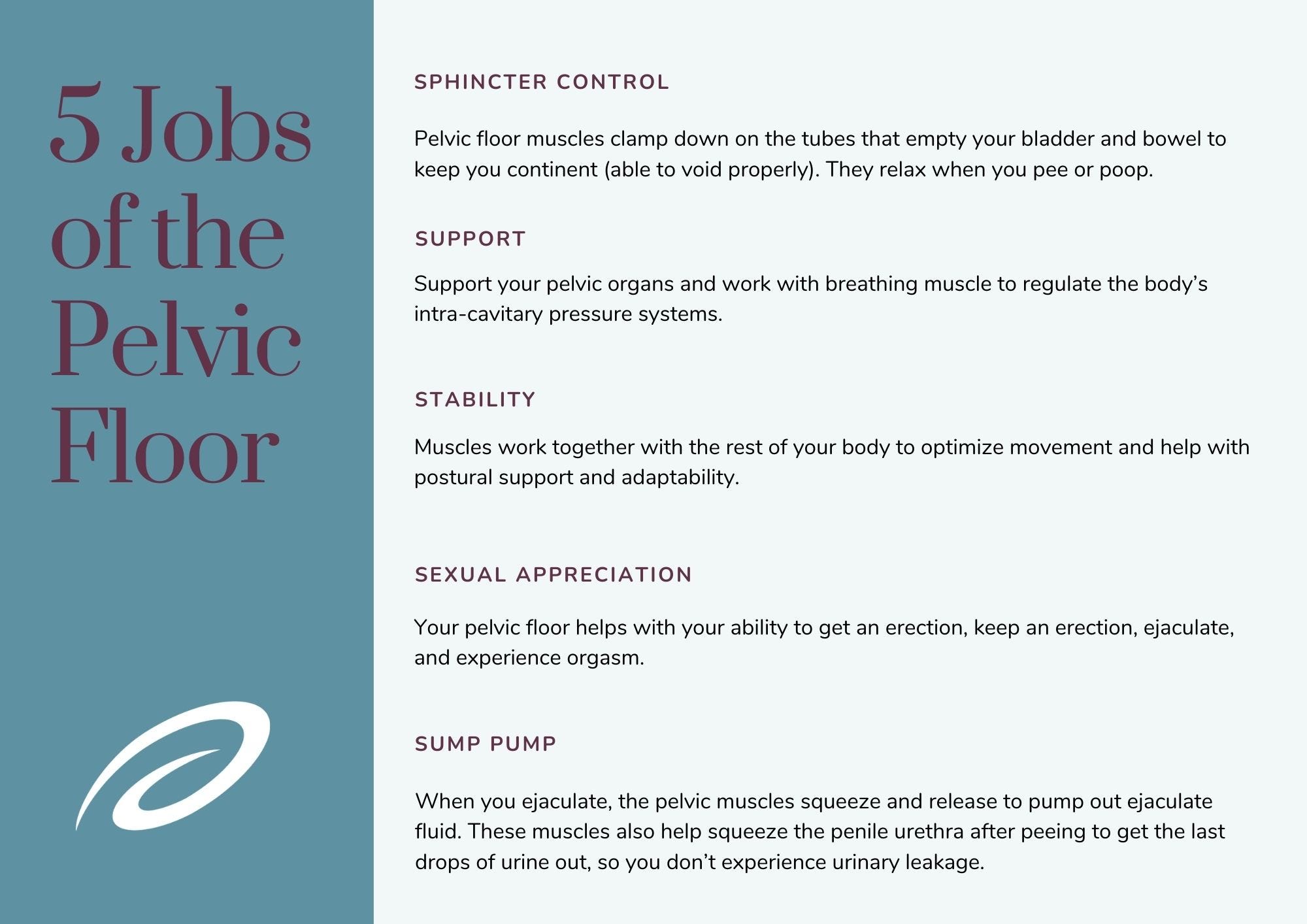
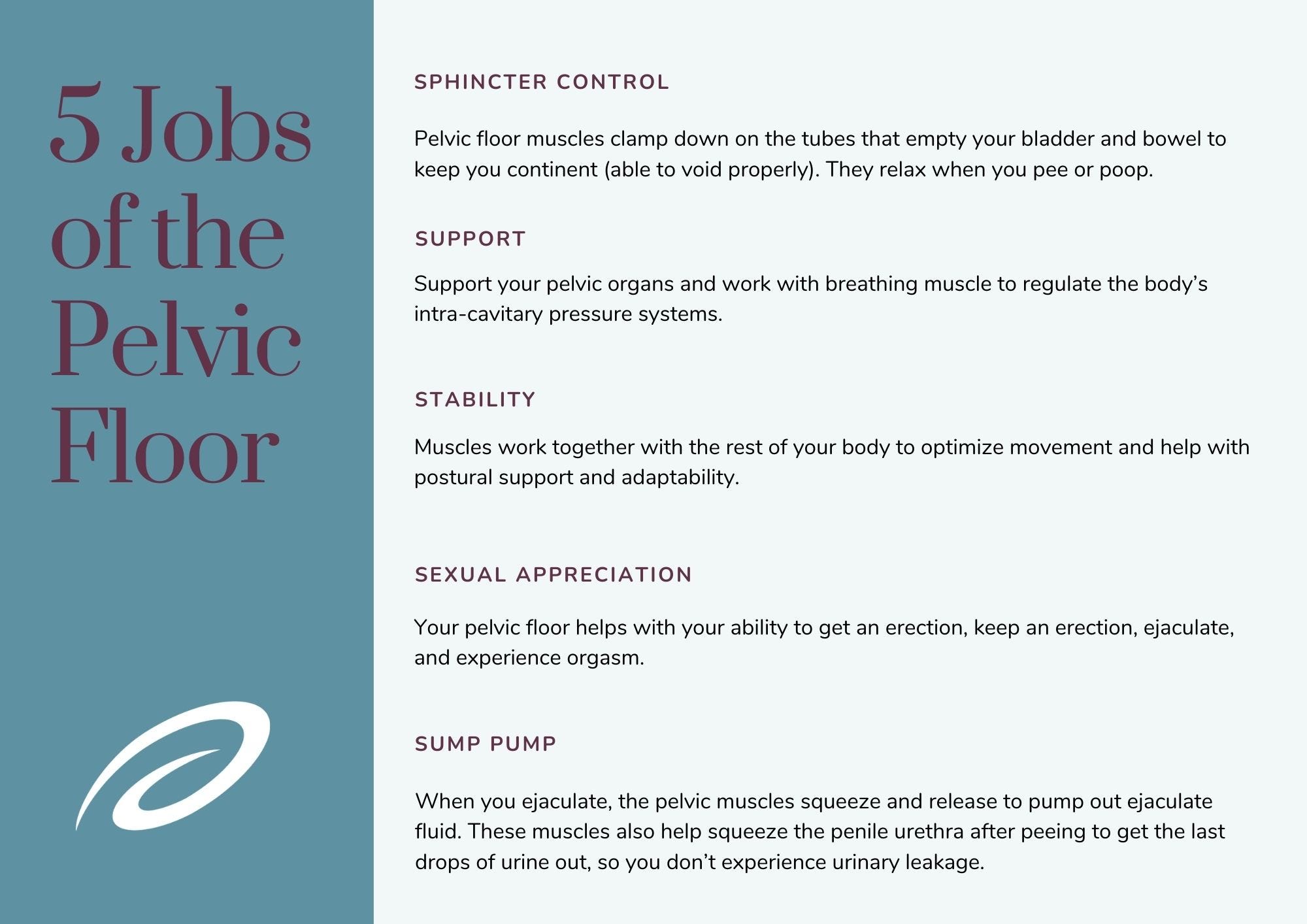
The pelvic floor serves many functions:
1. Sphincter control. The pelvic floor muscles clamp down on the tubes that empty your bladder and bowel to keep you continent (able to void correctly). They relax when you pee or poop.
2. Support. These muscles support your abdominal and pelvic organs and work with your breathing muscle to regulate your body's intracavitary pressure systems. When you cough, laugh, or sneeze, the pelvic muscles reflexively engage with the change in pressure from your abdomen into your pelvis.
3. Stability. The pelvic floor muscles work with the rest of your body to optimize movement and help with postural support and adaptability.
Like other skeletal muscles in your body, they constantly adjust and adapt to your activity and posture. Usually, you don't have to think about activating these muscles because many of these functions happen automatically—thank goodness!
4. Sexual appreciation. Yes, you read that right. Your pelvic floor (the muscles in addition to peripheral nerves, ligaments, blood vessels, spinal cord, and brain) helps with your ability to get an erection, keep an erection, ejaculate, and experience orgasm.
5. Sump pump. Like any plumbing system, you need to have a good urine flow. When you ejaculate, the pelvic muscles squeeze and release to pump out ejaculate fluid. These muscles also help squeeze the penile urethra after peeing to get the last drops of urine out so you don't experience urinary leakage.
What Causes Pelvic Floor Dysfunction & Incontinence in Males?
The most common causes for changes in bladder function and urinary continence mechanisms are the result of a disease, condition, or injury that alters the nerves or supporting organs involved with continence mechanisms, including:
-
Diabetes
-
Pulmonary conditions like asthma, chronic obstructive pulmonary disease, and emphysema.
-
Neurological conditions such as stroke, Parkinson's disease, multiple sclerosis, and spinal cord injury.
-
Prostate surgeries that result in the removal of supporting structures or alter nerve function related to bladder and sexual function, such as benign prostate hypertrophy (BPH) procedures like TURP, which stands for transurethral resection of the prostate.
-
Prostate cancer treatments like radical prostatectomy or radiation. A radical prostatectomy removes the internal urethral sphincter located at the bladder neck and may impair the nerves that help with bladder continence and sexual function.
Other factors that can influence bladder function and continence control include:
- Medications. Medications, such as alpha-blockers, blood pressure medications, certain antihistamines, diuretics, and antidepressants can harm the bladder.
- Constipation. The rectum and bladder share the same space within the pelvis. Therefore, chronic constipation results in excessive stress and strain on the bladder and pelvic muscles, contributing to stress and urge urinary incontinence, nocturia, urgency, and frequency.
- Caffeine and alcohol intake. These are considered "natural" diuretics that chemically interact with your body to increase urine production.


Although there is no direct link to caffeine or alcohol causing urinary incontinence, it has been postulated that they may act as bladder and bowel irritants / stimulants, which may contribute to or exacerbate nocturia, urge incontinence, urgency, and frequency.
- Smoking. Nicotine has been shown to irritate the bladder muscle. In addition, smoking may lead to chronic coughing, which adds excessive stress and strain on the bladder and pelvic muscles, causing or exacerbating stress and urge urinary incontinence. (Not to mention the side effects of erectile dysfunction, yikes!)
- Sedentary lifestyle. Physical activity encourages your body to kick into gear, exerting effort beyond your typical baseline. Sitting on the couch clicking your TV remote doesn't count as physical activity. This is what we call sedentary behavior. Exercise is an intentionally scheduled, structured, and repetitive physical activity with the goal of upping your health and fitness game. Physical activity and exercise promote health and well-being, including lowering your risk of incontinence and erectile dysfunction.
What Are the Symptoms of Pelvic Floor Dysfunction in Males?
1 in 20 men experience concerns with urinary incontinence. Even though these concerns are common, you don't have to live with soggy cheerios and other pelvic floor dysfunction concerns that can show up as:
- Pain. This may cause secondary pelvic floor dysfunction but is not usually primary. This pain can be penile, testicular, scrotal, prostate, anorectal, lower back, or abdominal.
- Stress Urinary Incontinence. Stress incontinence is the involuntary loss of urine during physical or exertional activities. You may experience urine leakage when coughing, laughing, sneezing, heavy lifting, or jumping.
- Urge Urinary Incontinence. Urge incontinence is the involuntary loss of urine following a sudden, strong urge to urinate.
- Fecal Incontinence. Fecal incontinence is the experience of involuntary loss of stool with activity or following a sudden strong urge to have a bowel movement.
- Sexual Health Difficulties. Erectile dysfunction, premature ejaculation, or delayed ejaculation.
-
Constipation
-
Bladder pain or bladder spasms & pelvic pain.
-
Changes in urine stream (i.e., start/stop urination, hesitancy initiating stream, weak urine flow).
-
Nocturia (waking up more than once in the night to urinate).
-
Frequent hemorrhoids or pain with sitting.
-
Sexual pain (erection pain, during or after ejaculation, and pain during or after intercourse or masturbation).
-
Penile pain, testicular pain, or scrotal pain (or any changes in penile appearance or function.
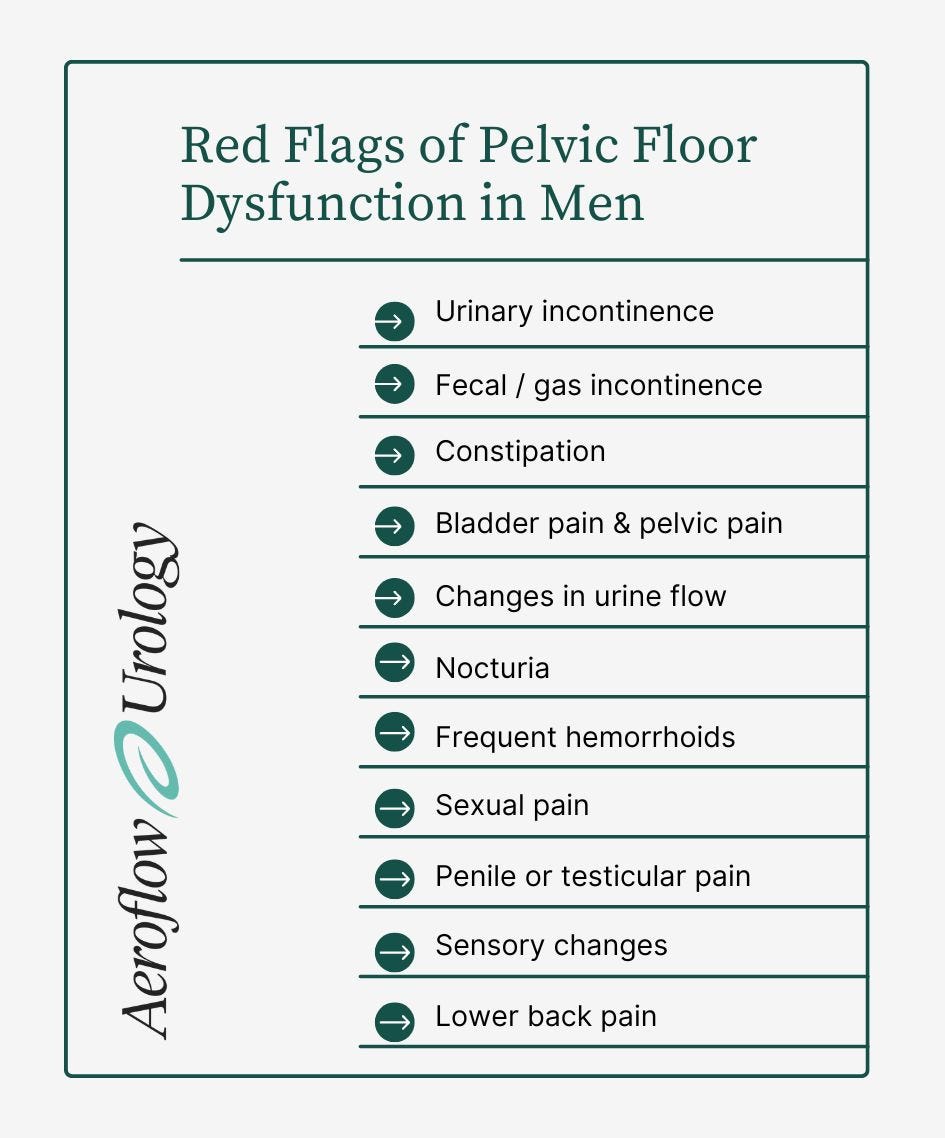
- Sensory changes like numbness, tingling, burning, and prickling sensations anywhere in the pelvic region, including sex organs.
- Lower back pain (there's a high correlation between low back pain and pelvic floor dysfunction).
How Can Males Strengthen Their Pelvic Floor Muscles?
There are multiple ways men can improve their pelvic floor muscle strength and decrease their risk of developing incontinence. These tips can also improve incontinence symptoms if they are already present.
Pelvic Floor Muscle Training
Pelvic floor muscle exercises, such as Kegel exercises, are for men too and can be integrated into your daily routine as part of your regular workout. If you use the correct muscles, pelvic floor exercises can significantly improve your pelvic floor strength.
Male Bladder Control Products
Stressed out about embarrassing incontinence issues? Incontinence products like adult pull-ons or male guards (male bladder pads) can help ease your anxiety because they protect against leaks and look like regular underwear. We also supply intermittent and other types of catheters if needed.
Did you know you can get male incontinence supplies for free with Aeroflow Urology if you qualify? That's right— fill out our Eligibility Form to get started and see if you can get your favorite incontinence products shipped to your doorstep in discreet packaging each month.
Biofeedback Therapy
Biofeedback is a tool used alongside pelvic floor muscle therapy. Biofeedback allows you to gain back control of your bladder. This type of therapy is also helpful after prostate surgery.
During biofeedback, electrical sensors give feedback to a monitoring system, and muscles are strengthened through repetition.
Pelvic Floor Therapy
The sooner you see a physical therapist or pelvic floor therapist, the better! Physical therapy and pelvic therapy are integral parts of the healthcare system and educate you on your pelvic and sexual health. Knowledge is power!
The more you understand how your body functions, the more empowered you will be to optimize your health, recognize future red flags, and feel more confident and comfortable in your body. Pelvic therapists also connect men to more resources, specialists, and health approaches that align with their values and goals.
Seeing a pelvic floor therapist is beneficial for many reasons. They can help strengthen your pelvic floor, improve incontinence symptoms, and keep your pelvic floor muscles strong and healthy. You can even do virtual pelvic floor therapy, so you won't need to leave your home.
Healthcare Provider Visits
If you need help managing your pelvic floor health, speak with your healthcare provider to make a plan. And remember-- you should never be ashamed to bring up issues with incontinence or pelvic floor health!
Minding Your Pelvic Floor
You're well on your way to taking charge of your pelvic health and urinary incontinence by learning how the pelvic floor and urinary incontinence are interconnected, recognizing red flags that need attention and specialized care, and starting to chart out treatment options you'd like to explore with your pelvic health team. Use our three tips to strengthen your pelvic floor muscles, and always pay attention down there!
One way to manage your pelvic floor is to use Aeroflow Urology to get free incontinence products. We offer incontinence supplies and catheters through Medicaid, Medicare, and some private insurance plans. To find out if you're eligible, simply fill out our Eligibility Form.
If you qualify, our Continence Care Specialists will contact you to answer questions, complete the necessary paperwork from your healthcare provider, and send you free samples of the products you're interested in.
After you choose your products, they'll be mailed to you in discreet packaging every month. We'll also send you helpful texts and email reminders when it's time to re-supply so you won't have to run to the store for extra products.
Dorey, G. (2006). Pelvic dysfunction in men: diagnosis and treatment of male incontinence and erectile dysfunction. John Wiley & Sons.
Haag, S. (2019). Understanding and treating Incontinence: what causes urinary incontinence and how to regain bladder control. OPTP.
Medications that contribute to incontinence/voiding dysfunction. (2021, May 15). Retrieved from https://www.nafc.org/glossary
Park, H.J., Park, C.H., Chang, Y., & Ryu, S. (2018). Sitting time, physical activity and the risk of lower urinary tract symptoms: a cohort study. BJU International, 122, 293-299. doi: 10.1111/bju.14147
Shields, K.M., Fox, K.L., & Liebrecht, C. (2018). Health professionals drug guide. Pearson.
Wyman, J.F., Burgio, K.L., & Newman, D.K. (2009). Practical aspects of lifestyle modifications and behavioural interventions in the treatment of overactive bladder and urgency urinary incontinence. International Journal of Clinical Practice, 63(8), 1177-1191. Doi: 10.1111/j.1742-1241.2009.02078.x
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.









