Key Takeaways:
- Illinois Medicaid covers incontinence supplies like diapers, pull-ons, underpads, and more for kids (age 4+) and adults with qualifying medical needs.
- Aeroflow Urology handles everything — we verify your coverage, work with your doctor, and ship products discreetly to your home every month for free if you qualify.
- We partner with most major Illinois Medicaid plans to help you get the supplies you need for free if you qualify.
Jump To:
Can You Get Incontinence Supplies Covered by Illinois Medicaid?
Which Incontinence Supplies May Be Covered?
Do You Qualify? Understanding Illinois Medicaid Eligibility for Incontinence Supplies
Navigating Medicaid Managed Care Plans in Illinois
How Aeroflow Urology Helps You Get Your Covered Supplies
Ready to See if You Qualify? Fill Out Our Eligibility Form
Where to Find Your Illinois Medicaid Insurance Information
How to Apply for Illinois Medicaid
What If You Don't Qualify? Other Options for Obtaining Incontinence Supplies in Illinois
Incontinence supplies like diapers and pull-ons shouldn’t cost money. If you're an Illinois Medicaid recipient, free incontinence supplies could be available to you or your loved one!
This blog will tell you how to determine your eligibility for free incontinence products through your Illinois Medicaid plan if you qualify, and how we can help you gather everything needed to get them delivered at no cost every month.
Can You Get Incontinence Supplies Covered by Illinois Medicaid?
Yes, if you qualify. Adults and children ages 4 and older may qualify for incontinence products through Illinois Medicaid and Aeroflow Urology.
Which Incontinence Supplies May Be Covered?
Eligible children in Illinois who are Medicaid or CHIP recipients may qualify to receive a combination of the following medical supplies and incontinence products:
- Pull-ups.
- Diapers
- Underpads (chux).
- Gloves
- Booster pads.
Eligible adults who are Illinois Medicaid beneficiaries may qualify to receive a combination of:
- Adult diapers (adult briefs).
- Adult pull-ons (protective underwear).
- Underpads (chux).
- Gloves
- Booster pads.
*Wipes are not currently available through insurance for Illinois Medicaid recipients.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Do You Qualify? Understanding Illinois Medicaid Eligibility for Incontinence Supplies
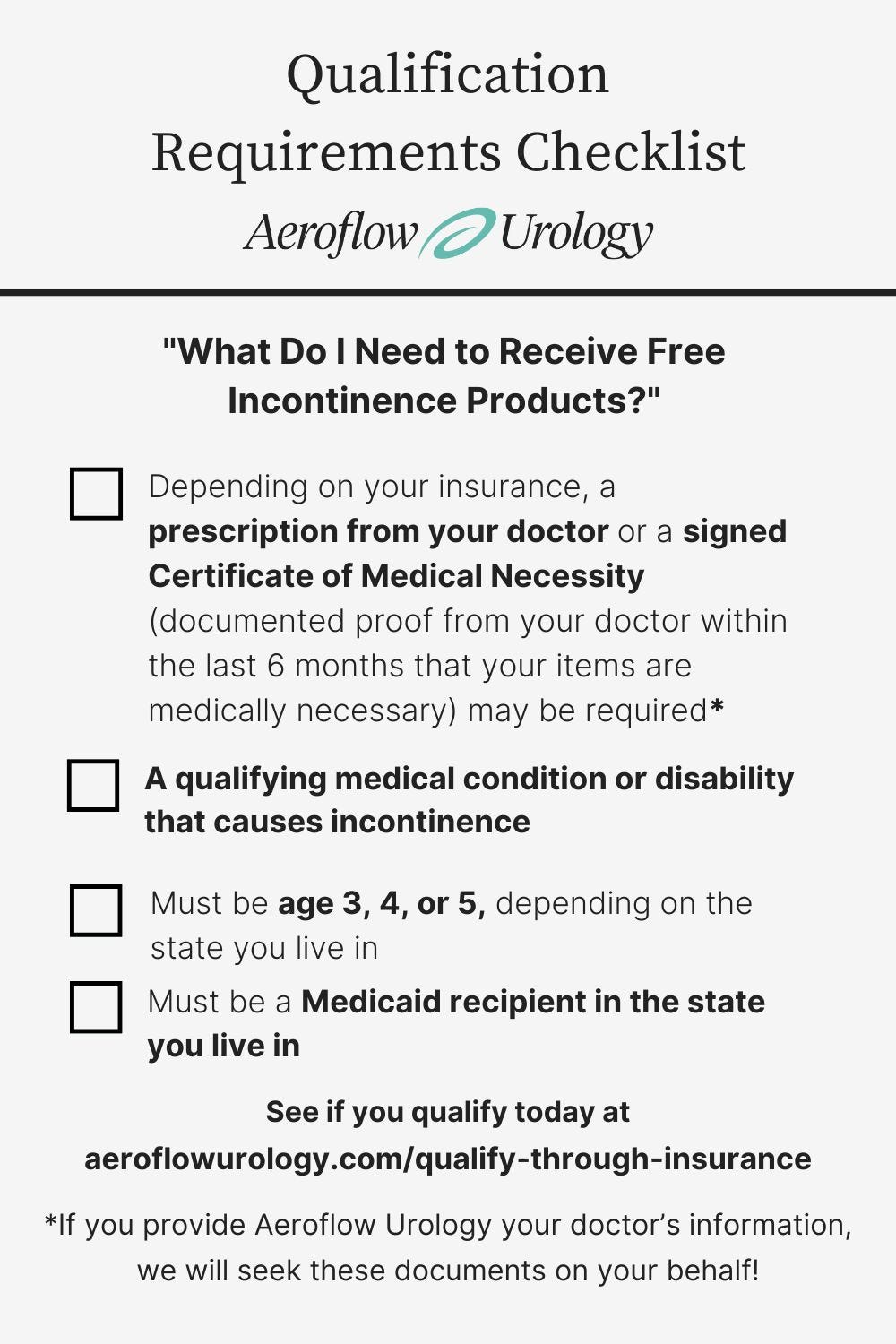
To receive free incontinence supplies through Illinois Medicaid with Aeroflow Urology, you may need to meet the following eligibility requirements (depending on your Medicaid program health insurance plan). Our Continence Care Specialists will help you gather all of the necessary information to make the process easy:
- Your medical reason for needing supplies (incontinence diagnosis with correlating disability or medical condition).
- An estimated number of incontinence products you need every day (i.e. 4 underpads, 5 diapers, etc.)
- A qualifying disability or medical condition that causes incontinence and is diagnosed by a healthcare professional, such as spina bifida, down syndrome, autism, etc.
- Must be 4 years of age or older.
- Must be an Illinois Medicaid recipient.
- Depending on your insurance, a signed Certificate of Medical Necessity (documented proof from your doctor within the last six months that your items are medically necessary) and / or a prescription from your healthcare provider.
Navigating Medicaid Managed Care Plans in Illinois
Medicaid-covered incontinence products are provided through Medicaid managed care plans that vary by state. In Illinois, Medicaid benefits, including incontinence supplies, are often managed through these provider names:
- Blue Cross Blue Shield.
- Countycare
- Meridian
- Molina
- Aetna Better Health.
- Humana Medicaid.
How Aeroflow Urology Helps You Get Your Covered Supplies
At Aeroflow Urology, we’ll verify your coverage and handle the paperwork required to receive incontinence products through your Illinois Medicaid benefits.
We are a durable medical equipment supplier (DME) that provides free, high-quality incontinence products from brands you can trust. Some of our customers’ favorite brands include:
- Attends
- Prevail
- Cuties
- TENA
Whether you need an adult brief, bladder control pad, pediatric diaper, or supplemental items, we can help you stay dry and protected with confidence with our wide variety of different product types and various absorbency levels. We work with you to help find the right mix of products to fit your individual needs.
Ready to See if You Qualify? Fill Out Our Eligibility Form
To see if you or your loved one qualifies for products, fill out our secure Eligibility Form.
Our form has been HiTrust-certified, so you know your information is secure! After we confirm your benefits and supplies, your Continence Care Specialist will contact you within 1-2 business days or after hearing back from your healthcare provider to go over sizing and product needs.
If you’re a caregiver, remember to fill out the form with your loved one’s information instead of your own!
Once your incontinence products are confirmed with your state Medicaid plan, we will discreetly package and ship your products directly to your home each month in unmarked boxes.
If you or your loved one uses incontinence products, you could save up to $630 each month through your Medicaid health plan and Aeroflow Urology!
Where to Find Your Illinois Medicaid Insurance Information
To complete our Eligibility Form and find out if you’re eligible for free incontinence supplies covered by Illinois Medicaid, you’ll need to have your insurance information ready. Insurance cards differ depending on the state you live in and the type of insurance you have (Illinois Medicaid or a Medicaid managed care plan), but you can find the following on your card:
- Full name of the insured person.
- The member ID number (Medicaid ID number).
- The plan name.
If you have questions regarding your insurance information, you can call the number on the card for beneficiaries.
How to Apply for Illinois Medicaid
If you are eligible for Illinois Medicaid, you can apply online and submit an application at https://abe.illinois.gov. If you have questions or need help applying, call the Health Benefits Hotline at 1-800-843-6154.
What If You Don't Qualify? Other Options for Obtaining Incontinence Supplies in Illinois
Visit Your Local Diaper Bank
If you or a loved one has incontinence and you don’t qualify for incontinence products through Medicaid, you may be able to go to your local diaper bank or a diaper drive to get free products. Low-income families may qualify for free diapers through a diaper program, along with other healthcare products, including those that protect against adult incontinence and pediatric incontinence.
Visit the Diaper Bank of Northern Illinois or the Diaper Bank of Southern Illinois to get your products. They may carry adult diapers, protective underwear, kid’s diapers, kid’s pull-ups, underpads, along with other incontinence supplies you might need.
Frequently Asked Questions
1. Does Illinois Medicaid have to be my primary insurance provider?
Incontinence products can be provided for any beneficiaries who have Illinois Medicaid as their primary or secondary provider.
2. How many supplies does Illinois Medicaid cover per month?
The number of briefs, pull-ups, and other supplies you receive will depend on what is allowed by Illinois' Medicaid plan as well as your prescription. Your Aeroflow Urology specialist will let you know exactly the quantity you are eligible to receive.
3. I have Illinois Medicaid, so why don’t I qualify for supplies?
You should have received an email outlining why you or your child was not approved for supplies. The reason could be due to the following: Aeroflow Urology is not in network with your Medicaid plan, or our contract may not allow us to provide the supplies you are requesting, you may not meet your insurance provider’s age requirement, incontinence supplies are not a covered item under your Medicaid plan, or you or your child’s disability may not be a qualifying condition under your plan.
4. I submitted my information to Aeroflow Urology. When will I know if I’m approved for free incontinence supplies?
One of our dedicated Continence Care specialists will contact you via phone or email within 1-2 business days of submitting your information. If it has been longer than this time frame, please give us a call at 844-276-5588 and we would be happy to check into your account and provide an update. Our office is open Monday-Friday 8am-5pm ET.
5. What about a prescription? Can Aeroflow help?
Illinois Medicaid requires a prescription in order to cover continence care products. If you do not have a prescription for you or your loved one, your Continence Care Specialist will reach out to your doctor directly for the paperwork.
6. I have Medicare. Why don’t I qualify for incontinence supplies?
Unfortunately, Medicare does not currently deem incontinence products as “medically necessary” so they do not cover supplies. However, they may cover your catheters.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.