Key Takeaways:
- Individuals with diabetes may experience urinary incontinence symptoms due to excessive thirst, obesity, medications, and nerve damage.
- Different treatment options can reduce symptoms of urinary incontinence.
IN THIS ARTICLE:
What Are the Causes of Urinary Incontinence In People With Diabetes? | What Types of Urinary Incontinence Can Develop From Diabetes? | How Do You Treat Urinary Incontinence In People With Diabetes? | How to Get Free Incontinence Products
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
Do you have diabetes and leak urine during the day or night? If so, you’re not alone.
Experiencing bladder issues, called urinary incontinence, is a common symptom of diabetes, and new research is showing just how strong the link between these conditions is. But managing both diabetes and urinary incontinence can be like solving two puzzles at once, which is why it’s essential to learn about their relationship and how to treat leakage.
Explore the profound link between diabetes and urinary incontinence and get practical, compassionate approaches to treating incontinence due to diabetes.
What Are the Causes of Urinary Incontinence In People With Diabetes?
Multiple studies have shown the prevalence of diabetes-related urinary incontinence (UI) symptoms in those with diabetes. This often unwanted side effect can develop for a few reasons.
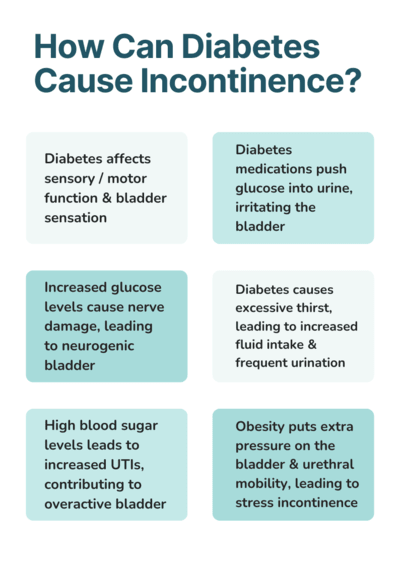
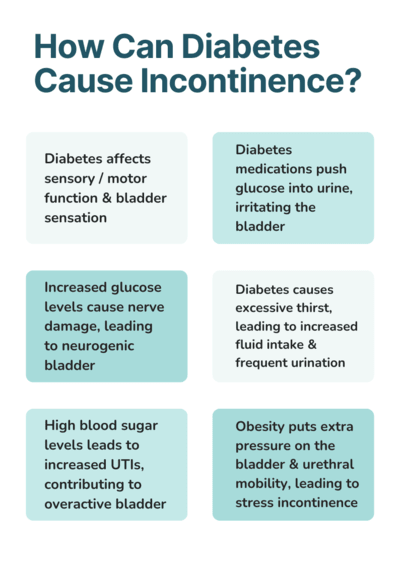
- Diabetes can affect sensory / motor function and bladder sensation, leading to frequent urination and urinary tract infections (UTIs).
- In an attempt to regulate high blood sugar levels, diabetes medications force glucose from the blood into the urine. When this happens, the bladder can become irritated, leading to UI.
- Increased glucose levels cause nerve damage (autonomic neuropathy), similar to peripheral neuropathy, which occurs when you lose sensation in your legs and feet. Autonomic neuropathy can cause you to develop a neurogenic bladder, resulting in UI. Neurogenic bladder is when the nerve connection between the bladder and brain is disrupted causing little to no sensation to need to empty your bladder. It can also cause bladder spasms leading to UI.
- Excessive thirst caused by diabetes contributes to UI. This is because drinking excessive amounts of fluid at one time increases pressure on the bladder, leading to more frequent urination. This also contributes to nocturia (waking up multiple times during the night to void your bladder), which disrupts sleep and irritates the bladder.
- High blood sugar levels contribute to frequent UTIs which contribute to an overactive bladder (OAB) and urinary frequency.
- Obesity can increase urinary incontinence through increased abdominal pressure causing increased pressure on the bladder and urethral mobility. This leads to urge and stress incontinence.
Other Contributing Risk Factors Leading to UI:
- Enlarged prostate glands.
- Constipation
- Genitourinary syndrome due to menopause / hormonal changes.
- Previous urinary tract surgery.
What Types of Urinary Incontinence Can Develop From Diabetes?
Different types of incontinence may develop from the symptoms of diabetes. These include:
Urge Incontinence: Having a sudden, intense urge to urinate, followed by an involuntary loss of urine. You may also need to urinate frequently, even during the night.
Stress Incontinence: Experiencing leakage when exercising, jumping, running, coughing, sneezing, laughing, etc.
Functional Incontinence: Failing to make it to the restroom in time due to immobility caused by conditions such as dementia, arthritis, or diabetic neuropathy.
Overflow Incontinence: The frequent or constant dribbling of urine due to not being able to empty your bladder completely.
Mixed Incontinence: Experiencing more than one of the above types of incontinence simultaneously.
How Do You Treat Urinary Incontinence In People With Diabetes?
In some cases, UI can only be managed. However, it can be treated in other cases and will go away with time and dedication. Some treatment methods even overlap with diabetes management to manage both conditions at once.
1. Urologist Appointment
When finding relief from diabetes and UI, evaluation by a urologist is key! Your urologist will:
- Evaluate your urine with a urinalysis.
- Identify the type of UI you have, ensuring that your treatment is specifically tailored to your needs.
- Establish a baseline of bladder function to help rule out pre-existing factors that may have gone unnoticed (i.e., incontinence from pregnancy, recurring UTIs, menopause, etc.).
If you’ve been recently diagnosed with diabetes, seek a referral to a urologist right away. Prevention is key!
2. Timed Voiding or Bladder Retraining
Bladder retraining, or timed voiding, is when you try to allow yourself to urinate only at certain time intervals and continue to prolong those intervals until they reach healthy levels (voiding every 2 hours is considered typical). This practice can help you regain bladder control over time.
3. Pelvic Floor Exercises or Pelvic Floor Physical Therapy
Pelvic floor exercises are more than just Kegel exercises! Including these in your exercise routine or finding a pelvic floor physical therapist (PFPT) can help improve your bladder function and lessen diabetic bladder symptoms by strengthening your bladder muscles. These exercises also improve sexual pleasure and help with pregnancy.
4. Medications
Anticholinergics are medications that are used to control leaks. These medications protect your bladder from the nerves firing too frequently and decrease the urethra from moving as often, preventing urge incontinence.
5. Intermittent Self-Catheterization
If your diabetes is causing urinary retention, your healthcare provider may suggest intermittent catheterization. Using an intermittent catheter can help you void your bladder, limiting the chance of overflow incontinence and damage to the bladder or kidneys.
6. Diet & Lifestyle Changes
A healthy diet and proper exercise play an important role in managing blood glucose levels and reducing pressure on your bladder. Eat plenty of fiber and incorporate foods that don’t irritate your bladder. Refrain from eating spicy, acidic, or dairy-based foods.
Drink 60-80oz of water daily to maintain proper hydration and reduce the risk of excessive thirst. Avoid alcohol, carbonated, and caffeinated drinks to control OAB. Avoiding constipation will help too!
Moderate physical activity 3-5 times a week is an excellent way to combat the risk of incontinence and maintain a healthy lifestyle.
7. Bladder Diary
A bladder diary can help you and your doctor track and evaluate the amount of fluids you are taking in and compare this to how often you urinate. This is an easy, non-invasive test to determine the condition of your bladder and what type of UI you may have.
8. Preparation
This may be the most important treatment option! You may not always be able to control your bladder, but you can control your preparation for the surprises that often come with UI.
Make sure you always have your incontinence supplies ready to use when you need them. Whether you need catheters to fully empty your bladder or bladder control pads to protect yourself from accidents, ensure that you have a plan (and supplies) to manage UI symptoms.
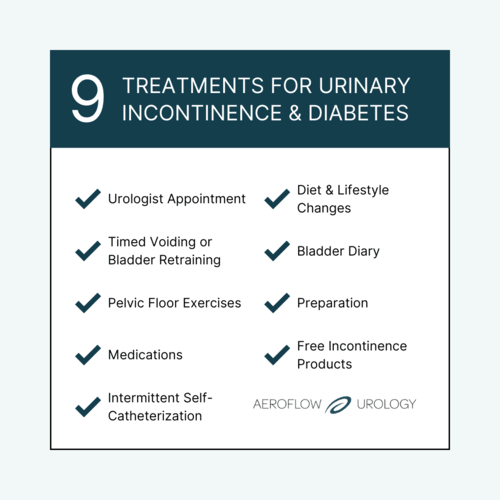
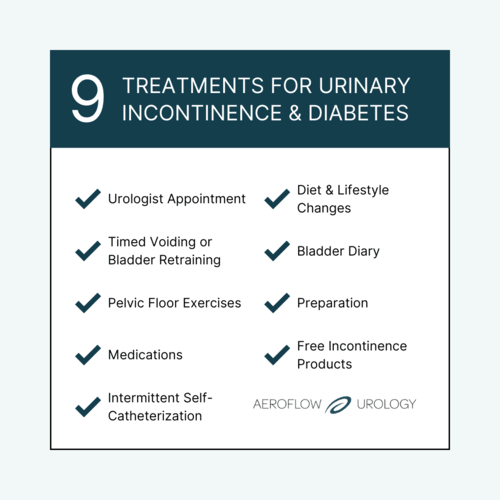
9. Free Incontinence Products
UI can steal sleep, cause stress, and keep you from living your best life. It may be common, but it does not have to be your normal!
At first, discussing your UI with a healthcare provider may feel embarrassing, but the reward of a diagnosis and treatment plan will be worth the brief uncomfortable moment.
If you have diabetes incontinence, you may qualify to receive FREE incontinence supplies through your Medicaid or Medicaid-managed care plan with Aeroflow Urology. Follow these steps to see if you qualify:
- Submit your insurance information through our secure Eligibility Form.
- Look for an email or text from Aeroflow Urology informing you of your eligibility.
- Get your free incontinence products!
Jump To: Top | Eligibility Form
References
Izci, Y., Topsever, P., Filiz, T. M., Çınar, N. D., Uludağ, C., & Lagro-Janssen, T. (2009). The association between diabetes mellitus and urinary incontinence in adult women. International Urogynecology Journal and Pelvic Floor Dysfunction, 20(8), 947–952. https://doi.org/10.1007/s00192-009-0888-8
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence issues.