This article was updated on 1/23/24.
During the COVID-19 pandemic, the US government declared a Public Health Emergency (PHE), which implemented many changes to systems nationwide. The PHE also altered how state Medicaid programs functioned. Certain Medicaid eligibility rules and policies were waived during the PHE to allow beneficiaries to keep their health care coverage over the course of COVID-19, making staying enrolled in a Medicaid plan simpler than ever before.
Since life has begun to return to normal, it unfortunately means the PHE waiver for Medicaid is coming to an end, leaving many people without CHIP or Medicaid coverage for things like incontinence supplies. If you’re one of the people wondering what to do if you’ve lost coverage for yourself or your loved one, don’t worry! This article will guide you to take the right steps to get your coverage back.
IN THIS ARTICLE:
Why Is Continuous Medicaid Coverage Ending?
When Does Continuous Medicaid Coverage End?
What Does the End of Continuous Medicaid Coverage Mean for Me?
How Do I Re-Enroll in CHIP or Medicaid Coverage?
Other Steps to Take if You Lose CHIP or Medicaid Coverage
Can I Get Free Incontinence Products With Medicaid & Aeroflow Urology?
Why Is Continuous Medicaid Coverage Ending?
Since the start of the coronavirus pandemic PHE in March 2020, states received more federal funding to be able to provide the public with continuous Medicaid enrollment.
Am I Covered?
Find Out In 2 Easy Steps
Discover the bladder control supplies covered by your Medicaid plan.
This continuous enrollment made it easier for Medicaid beneficiaries to maintain their coverage throughout COVID-19.
In December 2022, the federal government’s Consolidated Appropriations Act 2023 (CAA) took initiative to announce that the continuous enrollment provision will begin “unwinding” this spring.
When Does Continuous Medicaid Coverage End?
Starting April 1, 2023, the state you live in may resume its Medicaid recertification process after determining your eligibility for Medicaid coverage.
What Does the End of Continuous Medicaid Coverage Mean for Me?
This unwinding of the continuous coverage provision means that you and your loved ones may no longer be eligible for Medicaid. And you aren’t alone; according to the Kaiser Family Foundation (KFF), between 5 million and 14 million Medicaid beneficiaries across the country will lose coverage.
If your state finds that you are still eligible for Medicaid benefits, you still might run into administrative barriers and lose coverage. It all depends on the state you live in and its individual unwinding plan.
Unfortunately, while some state plans are prioritizing budget cuts and ending continuous enrollment faster, other states are putting people first. Certain states are helping beneficiaries continue their coverage by recertifying at a slower pace, and other states are making the Medicaid renewal process easier by reaching out to beneficiaries for updated eligibility requirements.
Note: Some states will not be reaching out to Medicaid recipients to announce when continuous coverage ends.
How Do I Re-Enroll in CHIP or Medicaid Coverage?
If you have lost Medicaid or CHIP coverage, you can reapply on your state's Medicaid or CHIP website or by calling your state Medicaid or CHIP office. This redetermination process may make you eligible for benefits.
Note: If you’ve already confirmed your Medicaid coverage for this year, nothing further is required. If you have not, please contact your state’s Medicaid office to do so.
Other Steps to Take if You Lose CHIP or Medicaid Coverage
There are a few things you can do if you face Medicaid of CHIP coverage losses this year and aren't eligible for reapplying.
- Appeal. If you lost Medicaid or CHIP and you think you shouldn’t have, you can try to appeal the decision with your state. You’ll need to request a hearing before your coverage end date, which will extend your coverage until your hearing date. If your coverage ends before your appeal because you missed the end date, you can reapply for Medicaid or CHIP in the interim. Contact your state Medicaid office to apply for an appeal.
- Look for marketplace coverage. If you’ve tried to appeal your Medicaid or CHIP coverage termination decision and you’ve reapplied for coverage but were denied and are still uninsured, you may want to look at different coverage options on the Healthcare Marketplace website.
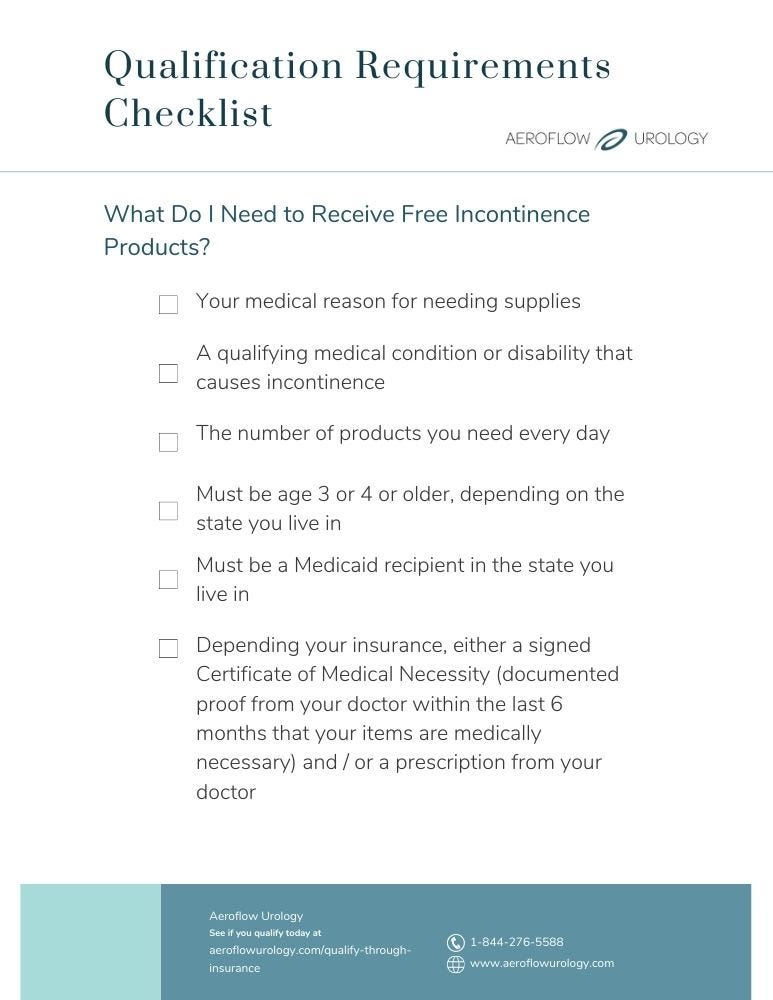
Can I Get Free Incontinence Products With Medicaid & Aeroflow Urology?
One of the best parts about receiving Medicaid health insurance is the free medical supplies you and your family members may qualify for.
Many individuals on low-income who have certain medical conditions or disabilities manage bladder and bowel control problems, requiring incontinence products that can be very costly out of pocket.
If you or your loved ones have conditions, such as spinal cord injury (SCI), autism, muscular dystrophy, cerebral palsy (CP), and more, you may qualify for incontinence products 100% covered by Medicaid.
We can supply you or your loved ones who qualify with the following products made by trustworthy brands, like TENA, Attends, and Prevail:
- Bladder control pads.
- Adult briefs.
- Adult pull-ons.
- Kids’ diapers and pull-ups.
- Other accessories for adults and children, like gloves, wipes, bed pads, and more.


Not only do you get your products completely free, but we also send free samples to you and your loved ones so you know your supplies suit your needs before ordering. We ship your incontinence supplies monthly and each time, your order ships free.
Here’s How It Works
1. Submit Form
Once you fill out our secure Eligibility Form, your coverage will be determined by your insurance plan and the state you live in. We never share your information with third parties and within 1-2 business days, one of our Continence Care Specialists will contact you to let you know if you qualify.
2. Choose Products
You'll be able to choose from our array of high-quality adult or pediatric incontinence products, such as pull-ups, bladder control pads, briefs, protective underwear from a personalized shopping list.
3. RX Received
After you're approved for coverage, we'll need to obtain a prescription from your healthcare provider. In order to receive your supplies faster, reach out to your provider’s office and let them know we'll be calling for a prescription on your behalf.
4. Shipped
Your selection of Medicaid-covered incontinence products will be shipped directly to your home in discreet packaging every month.
5. Restock
You'll get an email or text message reminder when it's time to restock your supplies.
Want free bladder and bowel control products? See if you qualify with us today.
References:
2022. (2022, May 10). Fiscal and Enrollment Implications of Medicaid Continuous Coverage Requirement During and After the PHE Ends. KFF. https://www.kff.org/medicaid/issue-brief/fiscal-and-enrollment-implications-of-medicaid-continuous-coverage-requirement-during-and-after-the-phe-ends/
Disclaimer:
Information provided on the Aeroflow Urology blog is not intended as a substitute to medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to continence care.