Key Takeaways:
- Identifying the type of incontinence you have can help in providing effective management.
- Incontinence can worsen mental health if left unaddressed.
- Talk therapy offers support for both the emotional and physical challenges of incontinence.
Check Your Eligibility
In Under 2 Minutes
Discover the incontinence products available through your insurance.
Jump To:
What Are the Types of Incontinence?
How Can Incontinence Cause Mental Health Conditions?
How Can Therapy Help Me Cope With Bladder Control Problems?
How Can I Find a Therapist for Incontinence?
What Are the Long-Term Benefits of Therapy for Incontinence?
How Else Can I Cope With Incontinence?
How Can I Get Free Bladder Control Supplies for Incontinence?
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
What Are the Types of Incontinence?
Incontinence is the loss of bladder and / or bowel control that leads to an unintentional loss of urine or feces. Urinary incontinence refers to the loss of urine, while fecal incontinence refers to the loss of fecal matter. In this article, we’ll focus mainly on urinary incontinence (UI).
There are many different types of UI, including:
- Stress incontinence: Leakage of urine when coughing, sneezing, laughing, bending over, lifting heavy objects, or exercising due to weakened pelvic floor muscles.
- Urge incontinence: Feeling the sudden and intense urge to empty your bladder frequently, resulting in urinary leakage.
- Overflow incontinence: Frequent or constant dribbling of urine due to the inability to empty your bladder completely.
- Functional incontinence: Having control over your voiding but leaking urine due to the inability to make it to the bathroom in time.
- Mixed incontinence: Experiencing more than 1 type of incontinence at the same time.
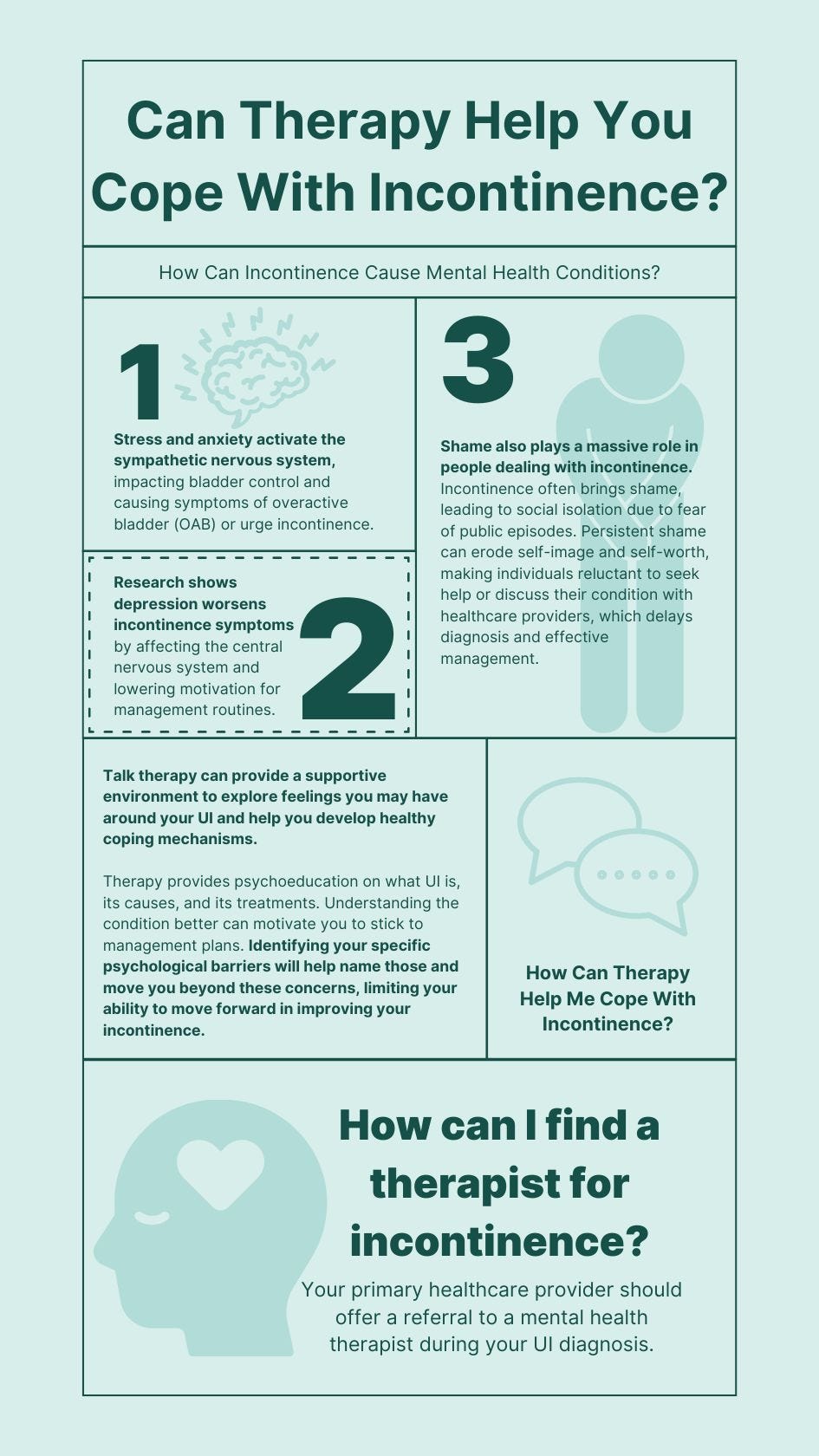
How Can Incontinence Cause Mental Health Conditions?
Incontinence can be embarrassing and cause depression and isolation. Mental health concerns, such as anxiety and stress, can worsen or exacerbate incontinence.
Stress and anxiety activate the sympathetic nervous system, which is part of the body’s fight-or-flight response. This activation can affect bladder control and lead to symptoms of overactive bladder (OAB) or urge incontinence.
Research has actually shown the connection between depression and incontinence. Depression may affect the central nervous system (CNS), which controls the bladder, thus worsening symptoms. Additionally, people with depression might be less motivated to maintain routines that manage or improve incontinence, such as pelvic floor exercises or regular toileting schedules.
Psychological factors can influence behaviors that exacerbate incontinence, such as increased intake of caffeine and / or alcohol, poor dietary habits (increased intake of bladder irritants), and irregular sleep patterns.
Shame also plays a massive role in people dealing with incontinence. With incontinence, shame often leads to social isolation for fear of having an incontinence episode while in public. Persistent shame can diminish a person’s self-image and self-worth and prevent people from seeking help or discussing their condition even with healthcare providers, which delays diagnosis and effective management.
How Can Therapy Help Me Cope With Bladder Control Problems?
All forms of therapy can be crucial for addressing the emotional and psychological aspects of managing incontinence. Specific talk therapy modalities include cognitive behavioral therapy (CBT), psychoeducation, Mindfulness-Based Stress Reduction (MBSR), supportive psychotherapy, solution-focused therapy, mindfulness, and group therapy.
Talk therapy can provide a supportive environment to explore feelings you may have around your UI and help you develop healthy coping mechanisms. Specific therapies, such as cognitive behavioral therapy (CBT), can assist in adopting behavioral strategies to manage incontinence better, such as:
- Bladder training.
- Scheduled toilet trips.
- Techniques to manage urgency.
- Diaphragmatic breathing and relaxation techniques.
Talk therapists may also suggest group therapy situations or support groups to help you feel connected and realize that you are not alone.
Talk therapy can also help address common misconceptions about incontinence. For example, incontinence is a normal part of the aging process. Talk therapy can assist you with ideas around incontinence being common, not normal, and that there are ways to improve your symptoms. Therapy can also provide a space for you to learn that incontinence is prevalent, that you are not alone, and that isolation and shame can limit the improvement of UI symptoms.
Talk therapists can also shed light on the fact that UI is not just a physical or medical issue. There are biopsychosocial influences on UI. Talk therapy can help you extrapolate the different causes or influences on UI, addressing problems holistically. This myth-busting empowers you to fight for answers and support for your UI.
Therapy provides psychoeducation on what UI is, its causes, and its treatments. Understanding the condition better can motivate you to stick to management plans. Identifying your specific psychological barriers will help name those and move you beyond these concerns, limiting your ability to move forward in improving your incontinence.
Talk therapy can provide coping mechanisms to combat interference with treatment modalities, maintain routines, and keep appointments. Setting realistic goals and having realistic expectations is crucial in addressing UI. Talk therapy can assist you in creating a strategic, achievable, creative plan specific to your unique needs. Talk therapy can also boost self-esteem, empowering you with tools to improve your UI and optimize your quality of life.
How Can I Find a Therapist for Incontinence?
Your primary healthcare provider should offer a referral to a mental health therapist during your UI diagnosis. It is up to you to accept the referral and go to therapy. However, your primary provider can easily discuss the importance of a mental health therapist.
Having a mental health therapist on site, ready to have even a brief conversation about UI, can be powerful. For those who are not familiar with therapy, talk therapy may feel scary, vulnerable, and even unnecessary if your culture is not supportive of therapy. It is important to include mental health therapy as part of the UI treatment plan when discussing treatment modalities.
What Are the Long-Term Benefits of Therapy for Incontinence?
Once shame, embarrassment, and anxiety are out of the way, and the realization that you don’t have to suffer in silence is clear, you may feel angry and upset that no one told you that before. This may cause a reaction to not let anyone else suffer from your symptoms.
Long-term benefits of talk therapy for incontinence may include you becoming a spokesperson for UI and telling everyone you know that incontinence is common, that there are treatment options, and that people don’t have to deal with this alone.
The tools provided during talk therapy may continue to serve as life-long skills you can implement. The confidence you may find after talk therapy can spill over into other areas of your life, empowering you to take on other concerns that might have felt embarrassing.
How Else Can I Cope With Incontinence?
- Remember that you are not alone!
- Talk to a trusted friend first and explain how you are feeling.
- Talk to a trusted healthcare provider about your symptoms.
- Make simple lifestyle changes, like eating fewer bladder irritants and decreasing alcohol and caffeine consumption.
- Avoid constipation by eating a diet full of fiber and whole foods.
- Increase your overall physical activity to help decrease UI symptoms and do pelvic floor muscle exercises, such as kegel exercises.
- Speak with your healthcare provider about medications for UI, such as oxybutynin.
- Try sacral nerve stimulation with a pelvic floor physical therapist or healthcare provider.
- See a pelvic floor physical therapist for pelvic floor physical therapy to strengthen your pelvic floor, decrease urine leakage, and increase the strength of your bladder muscle.
- Search the internet for statistics about UI and trusted, legitimate websites of organizations that dedicate their pages to incontinence.
- Search Facebook for Facebook groups, like the Aeroflow Urology Adult Facebook Support Group, to become part of those dedicated to discussing UI.
- Schedule an appointment to discuss your concerns about incontinence with your provider only. Dedicate this appointment to discussing incontinence and then prepare for your visit by writing down specific questions and / or concerns. Think about your goals for this visit and goals for your incontinence.
References
Stickley A, Santini ZI, Koyanagi A. Urinary incontinence, mental health and loneliness among community-dwelling older adults in Ireland. BMC Urol. 2017 Apr 8;17(1):29. doi: 10.1186/s12894-017-0214-6. PMID: 28388898; PMCID: PMC5385037.
Baker J, Costa D, Nygaard I. Mindfulness-based stress reduction for treatment of urinary urge incontinence: a pilot study. Female Pelvic Med Reconstr Surg. 2012 Jan-Feb;18(1):46-9. doi: 10.1097/SPV.0b013e31824107a6. PMID: 22453268.
Long JE, Khairat S, Chmelo E, Palmer MH. Mind over bladder: Women, aging, and bladder health. Geriatr Nurs. 2018 Mar-Apr;39(2):230-237. doi: 10.1016/j.gerinurse.2017.09.003. Epub 2017 Oct 16. PMID: 29042069.
Amuzu BJ. Nonsurgical therapies for urinary incontinence. Clinical obstetrics and gynecology. 1998 Sep 1;41(3):702-11.
Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, Haythornthwaite JA. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014 Mar;174(3):357-68. doi: 10.1001/jamainternmed.2013.13018. PMID: 24395196; PMCID: PMC4142584.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.