Key Takeaways:
- Ohio Medicaid covers incontinence supplies — like diapers, pull-ons, underpads, and more — for kids (age 3+) and adults with qualifying medical conditions.
- Aeroflow Urology makes the process easy: we verify your medical coverage, work with your doctor, and ship products discreetly to your home every month for free (with qualified coverage).
- We partner with most major Ohio Medicaid plans to help you get the incontinence supplies you need at no cost if you qualify.
Jump To:
Can You Get Incontinence Supplies Covered by Ohio Medicaid?
Which Incontinence Supplies May Be Covered?
Do You Qualify? Understanding Ohio Medicaid Eligibility for Incontinence Supplies
Navigating Medicaid Managed Care Plans in Ohio
How Aeroflow Urology Helps You Get Your Covered Supplies
Ready to See if You Qualify? Fill Out Our Eligibility Form
Where to Find Your Ohio Medicaid Insurance Information
How to Apply for Ohio Medicaid
What If You Don't Qualify? Other Options for Obtaining Incontinence Supplies in Ohio
Did you know that if you qualify, you could get incontinence supplies at no cost through Ohio Medicaid? If you or your loved one needs products like diapers, pull-ons, or underpads, you could be eligible to receive them if you meet certain requirements.
This article breaks down how to find out if you qualify and explains how Aeroflow Urology can help with the process — like handling the paperwork, coordinating with your doctor, and getting your supplies shipped discreetly to your home each month.
Can You Get Incontinence Supplies Covered by Ohio Medicaid?
Yes, if you qualify. Ohio Medicaid provides coverage for medically necessary incontinence products for eligible children (ages 3+) and adults.
Which Incontinence Supplies May Be Covered?
Eligible children (ages 3+) with Ohio Medicaid may qualify to receive a combination of the following medical supplies and incontinence products:
- Pull-ups.
- Diapers
- Underpads (chux).
- Gloves
- Booster pads.
Eligible Ohio Medicaid adults may qualify to receive a combination of:
- Adult diapers (adult briefs).
- Adult pull-ons (protective underwear).
- Underpads (chux).
- Gloves
- Booster pads.
*Unfortunately, wipes are not covered for Medicaid recipients in Ohio.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
Do You Qualify? Understanding Ohio Medicaid Eligibility for Incontinence Supplies
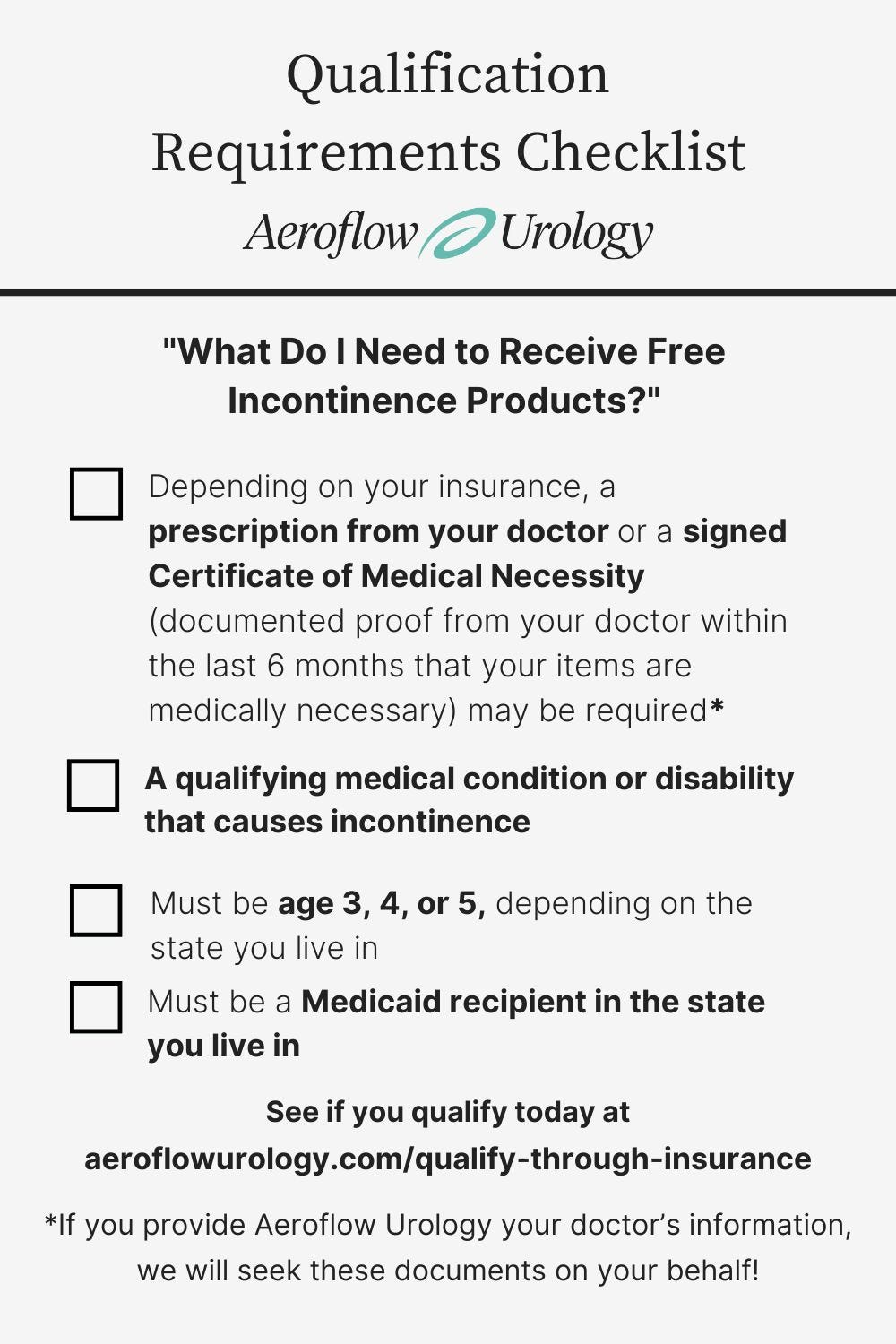
To get free incontinence supplies through Ohio Medicaid with Aeroflow Urology, you need to meet certain requirements based on your Medicaid plan. A dedicated Continence Care Specialist at Aeroflow Urology will help you collect everything you need to make the process easy:
- Your medical reason for needing supplies (incontinence diagnosis with correlating disability or medical condition).
- The estimated amount of incontinence supplies needed per day (i.e. 4 bladder control pads, 2 disposable underpads).
- A qualifying disability or medical condition that causes incontinence and is diagnosed by a healthcare professional, such as autism, Parkinson’s disease, Alzheimer’s disease, spina bifida, etc.
- Must be 3 years of age or older.
- Must be an Ohio Medicaid recipient.
- Depending on your insurance, a signed Certificate of Medical Necessity (documented proof from your doctor within the last 6 months that your items are medically necessary) and / or a prescription from your healthcare provider.
Navigating Medicaid Managed Care Plans in Ohio
Medicaid-covered incontinence products are provided through managed Medicaid plans that vary by state. In Ohio, Medicaid benefits, including incontinence supplies, are often managed through these provider names, known as Medicaid managed care plans:
- United Healthcare.
- Molina
- Buckeye Community Care.
- Paramount Advantage.
- Caresource
- Humana
- Anthem
- Amerihealth Caritas.
How Aeroflow Urology Helps You Get Your Covered Supplies
At Aeroflow Urology, we believe continence care products shouldn't come at a cost — because they're essential for your health, comfort, and quality of life. That's why we:
- Send you free samples of products so you can find your perfect fit.
- Ship your supplies quickly in discreet packaging directly to your home.
- Send you reminders when it's time to refill your products so you don't run out.
- Take the hassle out of determining whether or not you qualify under Ohio Medicaid.
The process is simple and the best part is you don't need to leave your house (unless you need a prescription from your healthcare provider). In fact, it all happens through your mobile device or computer.
To get started, just fill out our secure Eligibility Form.
We don't share your information with anyone else, and after confirmation of benefits and supplies, we'll contact you as soon as we hear back from your healthcare provider.
Ready to See if You Qualify? Fill Out Our Eligibility Form
To see if you or your loved one qualifies for products, fill out our secure Eligibility Form.
Our form has been HiTrust-certified, so you know your information is secure! After we confirm your benefits and supplies, your Continence Care Specialist will contact you within 1-2 business days or after hearing back from your healthcare provider to go over sizing and product needs.
If you’re a caregiver, remember to fill out the form with your loved one’s information instead of your own!
Once your incontinence products are confirmed with your Ohio Medicaid plan, we will discreetly package and ship your products directly to your home each month in unmarked boxes.
If you or your loved one uses incontinence products, you could save up to $630 each month through your Medicaid health plan and Aeroflow Urology!
Where to Find Your Ohio Medicaid Insurance Information
To complete our Eligibility Form and find out if you’re eligible for free incontinence supplies covered by Ohio Medicaid, you’ll need to have your insurance information ready. Insurance cards can look different depending on your plan — whether you have Ohio Medicaid or a managed care plan — but here’s what to look for on your card:
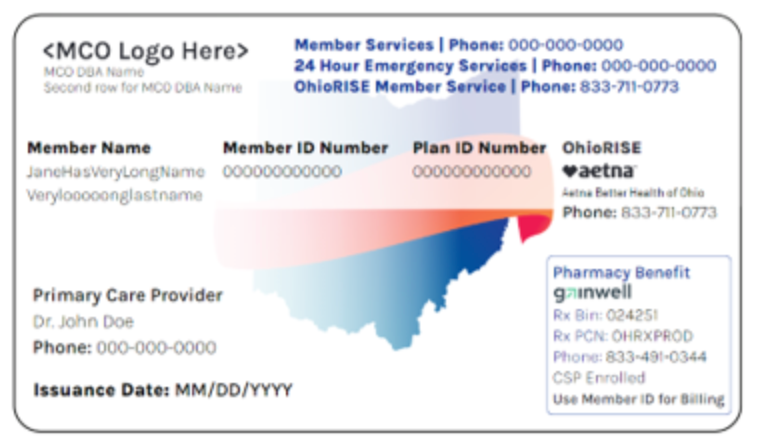
- Full name of the insured person.
- The member ID number (Medicaid ID number).
- The plan name.
If you have questions regarding your insurance information, you can call the number on the card for beneficiaries.
How to Apply for Ohio Medicaid
To find out if you are eligible for Ohio Medicaid, visit benefits.ohio.gov and submit your application online.
If you have questions or need help applying, you can call the Ohio Medicaid Consumer Hotline at (800) 324-8680.
What If You Don't Qualify? Other Options for Obtaining Incontinence Supplies in Ohio
If you or a loved one has incontinence but does not qualify for free supplies through Ohio Medicaid, you may still have options. Local diaper banks and community diaper drives often provide free incontinence products.
These programs support low-income families and offer a variety of supplies, such as adult diapers, protective underwear, kids’ diapers and pull-ups, underpads, and other helpful products for managing incontinence.
Some diaper banks in Ohio include:
- Diaper Bank of Greater Cleveland.
- Stark County Diaper Bank.
- Columbus Diaper Bank.
- Sweet Cheeks Diaper Bank.
Frequently Asked Questions
1. Does Medicaid have to be my primary insurance provider?
Incontinence products can be provided for any beneficiaries who have Ohio Medicaid as their primary or secondary provider.
2. How many supplies does Ohio Medicaid cover per month?
The number of briefs, pull-ups, and other supplies you receive will depend on what is allowed by your Ohio state Medicaid plan as well as your prescription. Your specialist will let you know exactly the quantity you are eligible to receive.
3. I have Ohio Medicaid – so why don’t I qualify for supplies?
You should have received an email outlining why you or your child was not approved for supplies. The reason could be one of the following: Aeroflow Urology is not in network with your Medicaid plan, or our contract may not allow us to provide the supplies you are requesting, you may not meet your insurance provider’s age requirement, incontinence supplies are not a covered item under your Ohio Medicaid plan, you or your child’s disability may not be a qualifying condition under your plan.
4. I submitted my information to Aeroflow Urology. When will I know if I’m approved for free incontinence supplies?
One of our dedicated Continence Care specialists will contact you via phone or email within 1-2 business days of submitting your information. If it has been longer than this time frame, please give us a call at 844-276-5588 and we would be happy to check into your account and provide an update. Our office is open Monday-Friday 8am-5pm ET.
5. What about a prescription? Can Aeroflow help?
Ohio Medicaid requires a prescription in order to cover continence care products. If you do not have a prescription for you or your child, your Continence Care Specialist will reach out to your doctor directly for the paperwork.
6. I have Medicare. Why don’t I qualify for incontinence supplies?
Unfortunately, Medicare does not currently deem incontinence products as “medically necessary” so they do not cover supplies. However, they may cover your catheters.
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.