Key Takeaways:
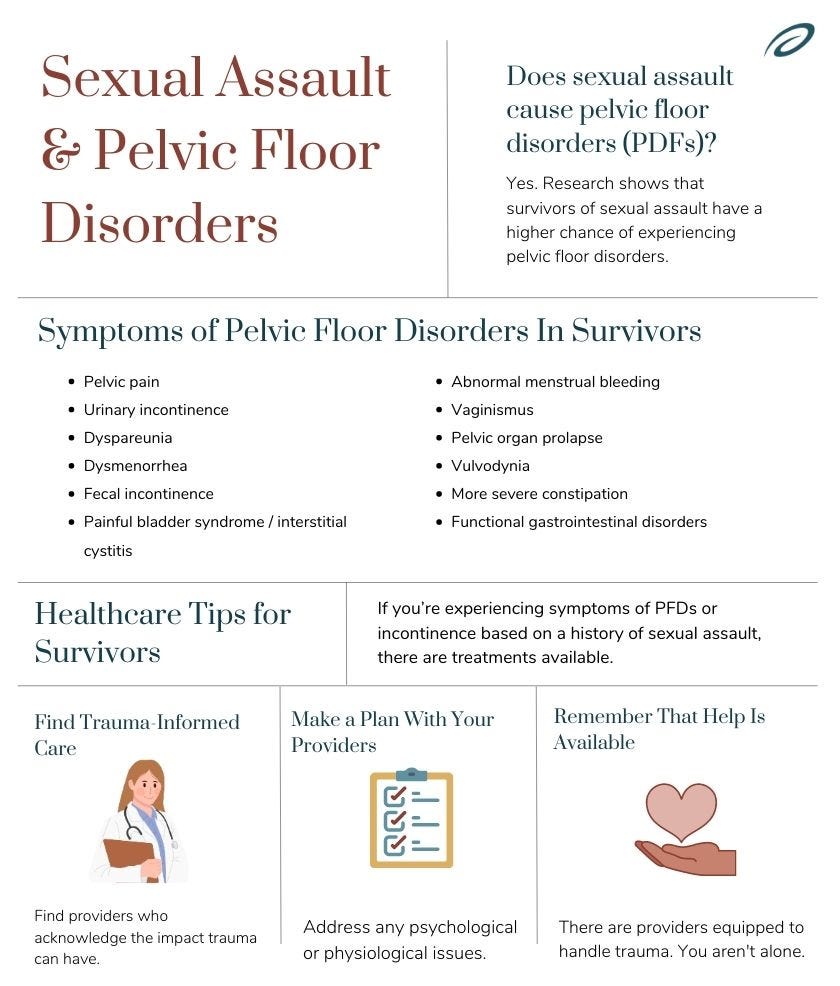
- Sexual assault can cause pelvic floor disorders and incontinence in some individuals.
- Women who have been sexually assaulted are 34% more likely to experience pelvic floor dysfunction symptoms.
- Treatments for incontinence after assault include finding trauma-informed care, making a treatment plan with providers, and remembering you are not alone.
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
Many psychological and physiological changes can develop in individuals who have experienced sexual assault.
Side effects like depression, anxiety, and post-traumatic stress disorder, have been acknowledged as legitimate in the healthcare community and our society.
But there is one set of conditions reported by survivors that hasn’t received much attention: Pelvic floor disorders.
Pelvic floor disorders can greatly impact people’s quality of life, especially if they’re healing from a trauma such as sexual assault. Read this article to find out how sexual assault and pelvic floor disorders, like incontinence, are related. Plus, get advice from our expert Medical Advisor on how to take care of your health after sexual assault.
A quick note to our readers: Although Aeroflow Urology and our Medical Advisors fully acknowledge that assault does not occur solely to females, and we are aware that males also experience sexual assault, there is an enormous gap in the availability of research to assess the association between male survivors of sexual assault and urological disorders. Therefore, this article is focused on female survivors and their symptoms.
What Are Pelvic Floor Disorders?
Pelvic floor disorders (PFDs) occur when your pelvic floor muscles or tissues are weakened or damaged. PFDs can happen to any person of any age, but they’re most common in older women.
Causes of PFDs include:
- Childbirth or pregnancy.
- Extra weight being placed on the pelvic floor muscles.
- Chronic constipation.
- Certain medications.
- Chronic forceful bowel movements (straining on pelvic floor).
- Aging
- Surgeries (hysterectomy, prostate, etc.).
Common symptoms of PFDs are:
- Vaginal pain.
- Pelvic organ prolapse (POP) (weakening of pelvic muscles, leading to a
- drop in pelvic organs causing vaginal bulging).
- Urinary retention (being unable to empty the bladder completely).
- Urinary or fecal incontinence.
- Pain while urinating.
- Constipation


What Is Incontinence?
Incontinence occurs when you lose control of your bladder or bowels.
Types of incontinence include:
- Stress Urinary Incontinence (SUI): Leaking urine when you cough, sneeze, laugh, have intercourse, exercise, bend over, or lift heavy objects.
- Urge Incontinence / Overactive Bladder (OAB): Feeling the sudden and intense urge to pee or urinating more than 8 times in 24 hours, resulting in leaks.
- Overflow Incontinence: Dribbling urine throughout the day due to urinary retention (leftover pee) in the bladder.
- Functional Incontinence: Having continence (control over your bladder) but leaking urine because of the inability to make it to the toilet due to medical conditions or other neurological conditions.
- Bowel / Fecal Incontinence: Leaking fecal matter.
- Mixed Incontinence: Experiencing one or more sets of incontinence symptoms at once (for example, leaking urine when you sneeze and peeing more than usual).
Some causes of incontinence include:
- Weak pelvic floor muscles.
- Aging
- Certain surgeries (prostate surgery, hysterectomy, etc.).
- Potty training delays or regression.
- Urinary tract infection (UTI).
- Hormonal changes (pregnancy, menopause, menstruation).
- Pregnancy or childbirth.
- Prostate problems (prostate cancer, benign prostate hyperplasia, etc.).
- Certain medications.
- Special needs (autism, Down syndrome, etc.).
- Medical conditions (spina bifida, spinal cord injury, etc.).
A healthcare provider or urologist may be able to diagnose which type of PFD or incontinence you have based on your symptoms. In some cases, both may be treatable and reversible with proper care. In other cases, a person may manage these issues throughout their lifetimes due to their unique condition.
The Connection Between Sexual Assault & Pelvic Floor Disorders
There is a connection between sexual assault, PFDs, and incontinence. These conditions are also referred to as “gynecological” or “urogynecological” symptoms.
Research has shown an association between sexual assault and the following symptoms of PFDs:
- Chronic pelvic pain.
- Painful bladder syndrome / interstitial cystitis.
- Functional gastrointestinal disorders (irritable bowel syndrome, irritable bowel disease).
- Non-specific chronic pain.
- Fibromyalgia
- Nocturnal enuresis (bedwetting).
- Psychogenic non-epileptic seizures (PNES) (seizures that are caused by psychological symptoms rather than epilepsy).
Other research has shown that women who have been sexually assaulted perceive symptoms of the following when compared to women who have not survived sexual assault:
- More severe fecal incontinence.
- More severe constipation.
- Impaired quality of life.
A recent 2020 systematic review and meta-analysis, which studied females of all ages with a history of sexual assault, explored whether assault increased the risk of gynecological morbidity (any issue with the reproductive system) compared to women without history of assault.
The study, which took 25 years to complete, found that women who were sexually assaulted had a 42% higher risk of experiencing gynecological symptoms compared to women who had no history of sexual assault.
Based on the results of the study, it can be concluded that the probability of a woman with a history of sexual assault having urogynecological symptoms is 36% compared to 27% in women without a history of sexual assault.
This means that women who have been sexually assaulted are 34% (or 1.34x) more likely to have symptoms that were found present in women included in the study.
Symptoms In Sexual Assault Survivors
These urogynecological symptoms from the study included:
- Pelvic pain.
- Urinary incontinence.
- Dyspareunia (genital pain that occurs before, during, or after intercourse).
- Dysmenorrhea (cramping and pelvic pain during menstruation).
- Abnormal menstrual bleeding.
- Vaginismus (tightening of vaginal muscles as a reaction to fear of vaginal penetration).
- POP
- Vulvodynia (chronic pain around the vulva with unidentifiable cause).
Why Do Symptoms Occur After Sexual Assault?
While there is no validated or conclusive theory to why urogynecological symptoms may occur in some survivors of sexual assault and not others, there are several theories around the physiological impacts of psychological and physical trauma brought on by:
- Early adverse childhood experiences.
- Life stressors.
- Life events.
- PTSD


These theories suggest that the following factors may contribute to PFDs and incontinence in sexual assault survivors:
- Organ changes: Adaptive and protective changes that may occur in survivors’ bodies can lead to changes in the organs, such as the bladder, bowel, uterus, and other associated structures and tissues.
- Post-traumatic stress disorder (PTSD): PTSD may develop in survivors which can put the body in a permanent “fight-or-flight” response, leading to physiological changes that can cause symptoms of urinary incontinence.
- Issues with immune and nervous systems: The immune and nervous system in the body of a survivor may get “amped up” due to accumulated psychological and physical stress on their biological state.
- Neuroendocrine maladaptation: Changes in survivors’ bodies, caused by chronic stress, can lead to the dysregulation of the hypothalamic pituitary adrenal axis.
- Psychosocial factors: Conditions experienced by some survivors, like depression and anxiety, may lead to chronically increased stress responses, involuntary muscle tension, and the previously mentioned amped up neuroimmune response.
- Neuroimmune pathological changes: Changes in survivors’ sympathetic nervous system may lead to “overprotection” and hyper-inflammatory states in the body.
- Neuroimmune “bioplastic” changes: Changes in survivors’ bodies which can result in peripheral and central nervous system (CNS) sensitization, as well as changes within the cortical body matrix which subserves the protection and regulation of the physical and psychological body.
Healthcare Tips for Sexual Assault Survivors With Pelvic Floor Disorders
If you’re experiencing symptoms of PFDs or incontinence based on a history of sexual assault, there are treatments available that can help you heal and end any incontinence symptoms you may have.
Find Trauma-Informed Care
It’s recommended by our experts that if you are a survivor of sexual assault– whether you’re experiencing urogynecological symptoms or not– you obtain care from trauma-informed providers.
These types of providers care for you as a whole and acknowledge the impact trauma can have. They are trained to identify signs of trauma and follow 5 principals: Safety, Choice, Collaboration, Trustworthiness, Empowerment.
Finding these types of doctors can also help avoid re-traumatization during care. Your clinicians should be people you can trust and feel safe with, as well as people who respect your boundaries and understand your unique needs.
You should seek out a team of the following types of trauma-informed healthcare providers:
- General practitioner: General healthcare provider.
- Urogynecologist: Surgeon who specializes in women’s pelvic floor disorders.
- Urologist: Doctor who specializes in reproductive and urological conditions.
- Pelvic floor physical therapist: Physical therapist who specializes in PFDs.
- Psychotherapist: Psychiatrist, psychologist, social worker, or counselor who specializes in different types of therapy.
Make a Plan With Your Providers
Once you’ve found trauma-informed healthcare professionals, you can make a plan to begin addressing any psychological or physiological issues that may be attributed to sexual assault.
You may also create a plan to treat or reverse your PDF / incontinence symptoms with a specialist like a pelvic floor physical therapist or urologist.
Everyone’s care after sexual assault is different, so depending on your most severe symptoms, your providers may want to tackle mental conditions before urinary conditions.
Remember That You Are Not Alone
Surviving sexual assault and managing the multitude of symptoms and effects that may develop afterward can be very challenging, but it’s important to remember that you are not alone.
Don’t Give up on Therapy
It may take a while to find a therapist or psychiatrist who is the right fit for you, but don’t give up!
Don’t Be Afraid to Use Bladder Control Products
It may feel embarrassing at first, but using bladder control products is one of the easiest way you can manage symptoms of incontinence. Products like women’s protective underwear and bladder control pads will keep you dry and confident.
You can check to see if you qualify for free bladder control products through Aeroflow Urology’s Eligibility Form.
Find Your Safe Space
It might be difficult to openly discuss your experience with sexual assault and incontinence, but having a support system in place is one of the best ways to heal, and talking about it gets easier with time.
How You Can Help
Sexual assault is a sensitive topic for many survivors, and for some, it’s not only the experience itself that carries weight. The immediate and long-term side effects that can present themselves after assault and other traumatic events are also delicate subjects, but they are acknowledged by our society, which may make speaking up about such effects and getting help easier for survivors.
Psychological and physiological changes, such as PTSD, dissociation, substance abuse, flashbacks, eating disorders, anxiety, self-harm, and more, have been correlated to sexual assault in healthcare and research spaces. PFDs and incontinence have been linked to sexual assault, but, as these types of urinary issues go, there is a stigma around openly discussing them. They’re seen as “embarrassing” or “shameful”-- to the point where some women report hiding their symptoms from healthcare providers and family members.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
By educating ourselves about PFDs and incontinence, and acknowledging that these effects of sexual assault can happen to anyone at any time in their lives, we will not only de-stigmatize the topics for the general public, but also create awareness for sexual assault survivors, making their healing process easier and improving their well-being.
If you have been sexually assaulted and wish to get help, you can text the Crisis Hotline or call the National Sexual Assault Hotline at 1-800-656-4673.
References
Hassam, T., Kelso, E., Chowdary, P., Yisma, E., Mol, B. W., & Han, A. (2020). Sexual assault as a risk factor for gynaecological morbidity: An exploratory systematic review and meta-analysis. European Journal of Obstetrics & Gynecology and Reproductive Biology, 255, 222–230. https://doi.org/10.1016/j.ejogrb.2020.10.038
Imhoff, L. R., Liwanag, L., & Varma, M. (2012). Exacerbation of Symptom Severity of Pelvic Floor Disorders in Women Who Report a History of Sexual Abuse. Archives of Surgery, 147(12), 1123. https://doi.org/10.1001/archsurg.2012.1144
Paras, M. L., Murad, M. H., Chen, L. P., Goranson, E. N., Sattler, A. L., Colbenson, K. M., Elamin, M. B., Seime, R. J., Prokop, L. J., & Zirakzadeh, A. (2009). Sexual Abuse and Lifetime Diagnosis of Somatic Disorders. JAMA, 302(5), 550. https://doi.org/10.1001/jama.2009.1091
Pelvic Floor Disorders (PFDs). (n.d.). Https://Www.nichd.nih.gov/. Retrieved March 1, 2023, from https://www.nichd.nih.gov/health/topics/pelvicfloor#:~:text=The%20most%20common%20PFDs%20are
Dworkin, E. R., Jaffe, A. E., Bedard-Gilligan, M., & Fitzpatrick, S. (2021). PTSD in the Year Following Sexual Assault: A Meta-Analysis of Prospective Studies. Trauma, Violence, & Abuse, 152483802110322. https://doi.org/10.1177/15248380211032213
DAVILA, G. W., BERNIER, F., FRANCO, J., & KOPKA, S. L. (2003). Bladder Dysfunction in Sexual Abuse Survivors. Journal of Urology, 170(2), 476–479. https://doi.org/10.1097/01.ju.0000070439.49457.d9
Mayson, B. E., & Teichman, J. M. H. (2009). The relationship between sexual abuse and interstitial cystitis/painful bladder syndrome. Current Urology Reports, 10(6), 441–447. https://doi.org/10.1007/s11934-009-0070-3
What is Trauma-Informed Care? (n.d.). Socialwork.buffalo.edu. https://socialwork.buffalo.edu/social-research/institutes-centers/institute-on-trauma-and-trauma-informed-care/what-is-trauma-informed-care.html#:~:text=The%20Guiding%20Values%2FPrinciples%20of%20Trauma%2DInformed%20Care&text=The%20Five%20Guiding%20Principles%20are
Disclaimer
Information provided on the Aeroflow Urology website is not intended as a substitute to medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.