Key Takeaways:
- Experiencing lower back pain and incontinence together may indicate a serious underlying issue, requiring proper understanding and treatment.
- Effective management often includes professional guidance, physical therapy, medication, and lifestyle changes such as exercise and diet adjustments.
- Aeroflow Urology offers support through personalized care and insurance-covered incontinence supplies, helping maintain dignity and ease management.
The tweaks, aches, and pains that come with lower back pain can be demotivating and distracting as is, but what happens when you throw incontinence into the mix?
Check Your Eligibility
In Less Than 2 Minutes
Discover the bladder control supplies covered by your insurance plan.
Experiencing these 2 things together often cause rushed trips to the bathroom and pain when moving, disrupting your quality of life.
More importantly, if you experience lower back pain and incontinence simultaneously, it may be a sign of a more serious underlying symptom. In this article, we’ll teach you how to manage your symptoms so you can return to doing the things you love.
Jump To:
Why Does Lower Back Pain Occur With Incontinence?
Types of Incontinence Related to Lower Back Pain
Spinal Disorders & Neurogenic Bladder Dysfunction
Cauda Equina Syndrome & Incontinence
Lower Back Pain & Incontinence In Women
How to Manage Lower Back Pain & Incontinence
INCONTINENCE PRODUCTS THROUGH INSURANCE:
Aeroflow Urology is in-network with many Medicaid and Medicaid-managed insurance plans and is accredited by Medicaid. Complete our Eligibility Form, and we’ll automatically check to see if your plan covers incontinence supplies. ***Must meet certain requirements to qualify.***
You will also receive the care and attention every person managing incontinence deserves: A personalized list of 100% insurance-covered incontinence supplies, a dedicated Continence Care Specialist you can contact during business hours, a user-friendly online portal for easy monthly reordering, and educational content.
Get the continence care you need with the dignity you deserve. Join the Aeroflow Urology family today! It only takes 5 minutes to get started.
What Is Lower Back Pain?
Lower back pain is common in the United States— it accounts for 264 million lost workdays in one year. Lower back pain occurs in the lower part of the back and spine. This area is called the lumbar spine region.
While some people experience acute lower back pain, lasting up to 3 months, some experience chronic lower back pain, which can last for longer.
If you have lower back pain, you may experience:
- Stiffness
- A decreased range of motion.
- Muscle spasms.
- Difficulty standing or sitting.
- Dull or aching pain down the back of the legs, also known as sciatica.
- Numbness in legs.
- Sharp pain in the lower back.
People develop lower back pain for a multitude of reasons, including:
- Herniation of a disk in the spine.
- Back structure problems, also known as spinal stenosis.
- Arthritis or osteoarthritis.
- Back strains, sprains, or fractures.
- Kidney stones or tumors.
What Is Urinary Incontinence?
Incontinence is when you lose the ability to control your bladder. It’s prevalent, and there are different types and causes of urinary incontinence.
Common causes of urinary incontinence are:
- Aging
- Prostate cancer.
- Obesity
- Urinary tract infections (UTIs).
- Giving birth.
- Certain medications.
Why Does Lower Back Pain Occur With Incontinence?
Our bodies are much more connected than we realize, so lower back pain and incontinence are often associated with one another.
The bladder and kidneys are located towards the lower abdomen, with back muscles and nerves sitting directly behind them. Because these areas are so close together, bladder conditions may cause pain in the back, and issues affecting the back muscles, spine, or nerves, can impact your bladder and lead to incontinence.
Types of Incontinence Related to Back Pain
Urinary Incontinence: This can occur when someone no longer has bladder control and has unintentional losses of urine.
Overactive Bladder (OAB): This type of incontinence occurs when you have a sudden urge to urinate that may lead to frequent bathroom trips or accidental leakage. If you have OAB and lower back pain together, it’s possible that you may be overweight, have prostate or kidney issues, or have cancer. Other symptoms you may experience with OAB and lower back pain include:
- Bloody or cloudy urine.
- The constant urge to pee.
- Pain in your lower abdomen.
- Pain / burning during voiding.
- Pain when ejaculating.
- Vomiting / nausea.
- Fever
- Inability to void urine or void completely.
Fecal Incontinence: Bowel incontinence is when you lose control of your bowels and fecal matter. This can occur alongside lower back pain if your
Overflow Incontinence: Overflow incontinence occurs when you’re unable to pass urine completely, otherwise known as urinary retention, and your urine “overflows” out of your urethra.
Stress Incontinence: Stress incontinence happens when urine leaks when you sneeze, cough, laugh, lift heavy objects, or exercise. This is due to stress being put on your bladder muscles. After giving birth, stress incontinence and lower back pain are both common in women.
Spinal Disorders & Neurogenic Bladder Dysfunction
Often spinal disorders associated with injuries that result in nerve damage are linked to Neurogenic bladder disorder (NBD), which refers to urination issues. Neurogenic is the nerve tissues that stimulate an organ or muscle to function correctly.
With NBD, the nerves that control the bladder and other muscles involved with urination may cause the bladder to be under or overactive.
When the nerves for bladder sensation or function become irritated, inflamed, or compressed, dysfunctions such as frequent urination, the sudden overwhelming urge to urinate, or involuntarily voiding the bladder may occur.
NBD is commonly caused by spinal cord injuries (SCI). Accidents that cause bruising or constrict blood flow along the spinal cord can damage the ability to transmit nerve signals.
Herniated discs, infections, lesions, lumbar tumors, and fractures along the spine can also cause back pain and damage to the spinal nerves leading to bladder dysfunction. These conditions may also cause Cauda Equina Syndrome (CES), a severe medical issue requiring immediate attention.
Cauda Equina Syndrome & Incontinence
Cauda equina syndrome (CES) is a condition that causes squeezing or compression in the cauda equina sac of nerves at the nerve roots or base of the spinal cord, resulting in lower back pain and urinary incontinence. As the nerves are pinched, they cannot properly function and may result in the involuntary loss of urine.
Cauda equina symptoms include weakness in the legs, numbness or tingling in the lower back and legs, and incontinence.
In some cases, cauda equina can be treated by surgically decompressing the spine, depending on the nerve tissue damage.
Lower Back Pain & Incontinence In Women
Depending on the cause of back pain or incontinence, symptoms may vary. For example, women often struggle with stress incontinence after giving birth and leak while participating in activities that add stress to the bladder, such as laughing, sneezing, or lifting a heavy object. However, kidney problems such as stones can also cause frequent urination or urge incontinence– when the urge to urinate suddenly strikes.
While studies show that the cause of back pain and incontinence is linked to weight gain or sedentary lifestyles in some patients, both conditions can also be caused by chronic illnesses like type 2 diabetes and arthritis.
When it comes to giving birth, 50% of women report stress urinary incontinence. In addition, postpartum back pain and incontinence may impact moms up to twelve months after their babies are delivered due to pelvic floor weakness.
Pelvic floor muscles often weaken due to the added stress of supporting a growing infant and supporting the body during labor. Once weakened, pelvic floor muscles are less able to function under increased pressure from the abdominal muscles during physical activities, leading to leaks. Pelvic floor muscles also play a role in spinal stability.
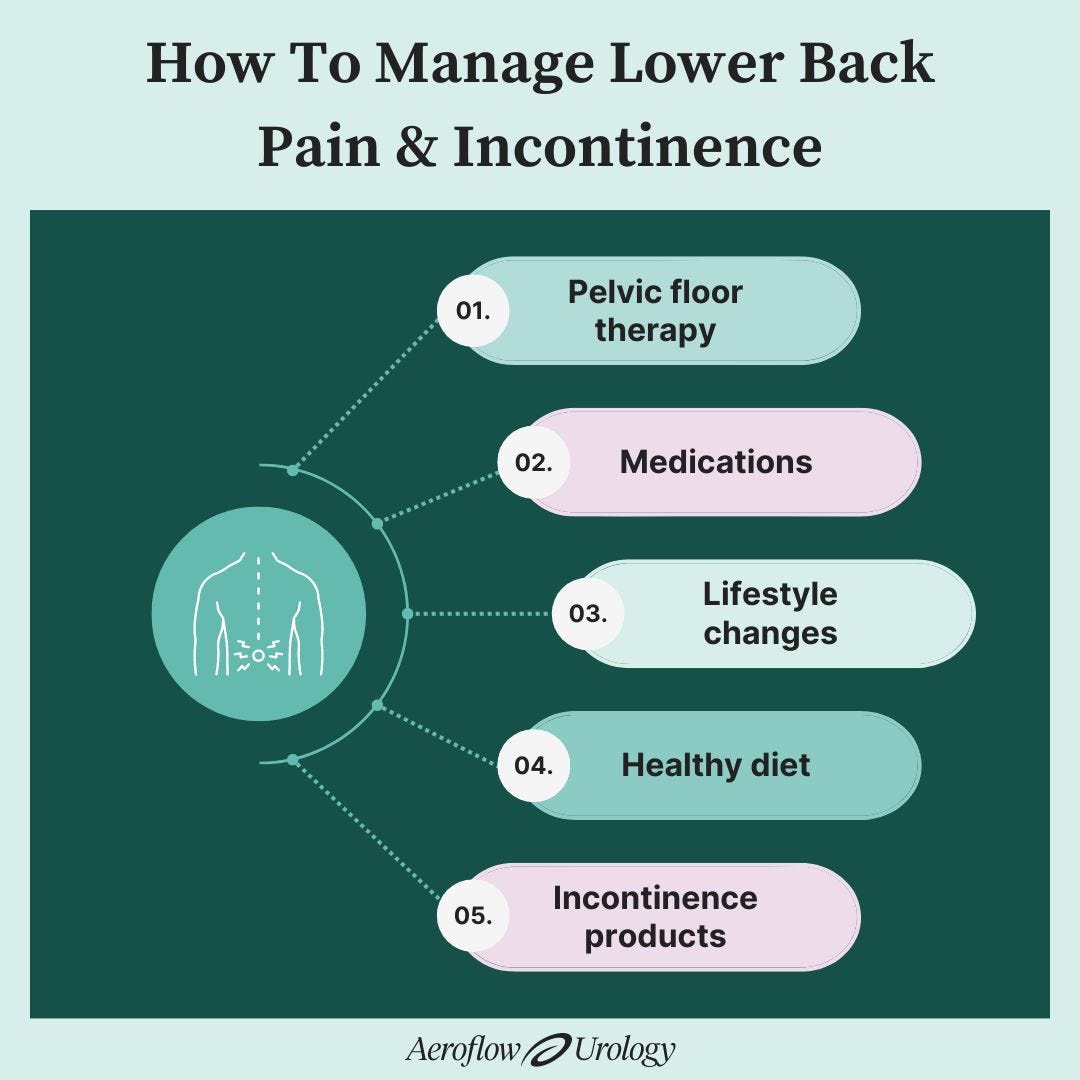
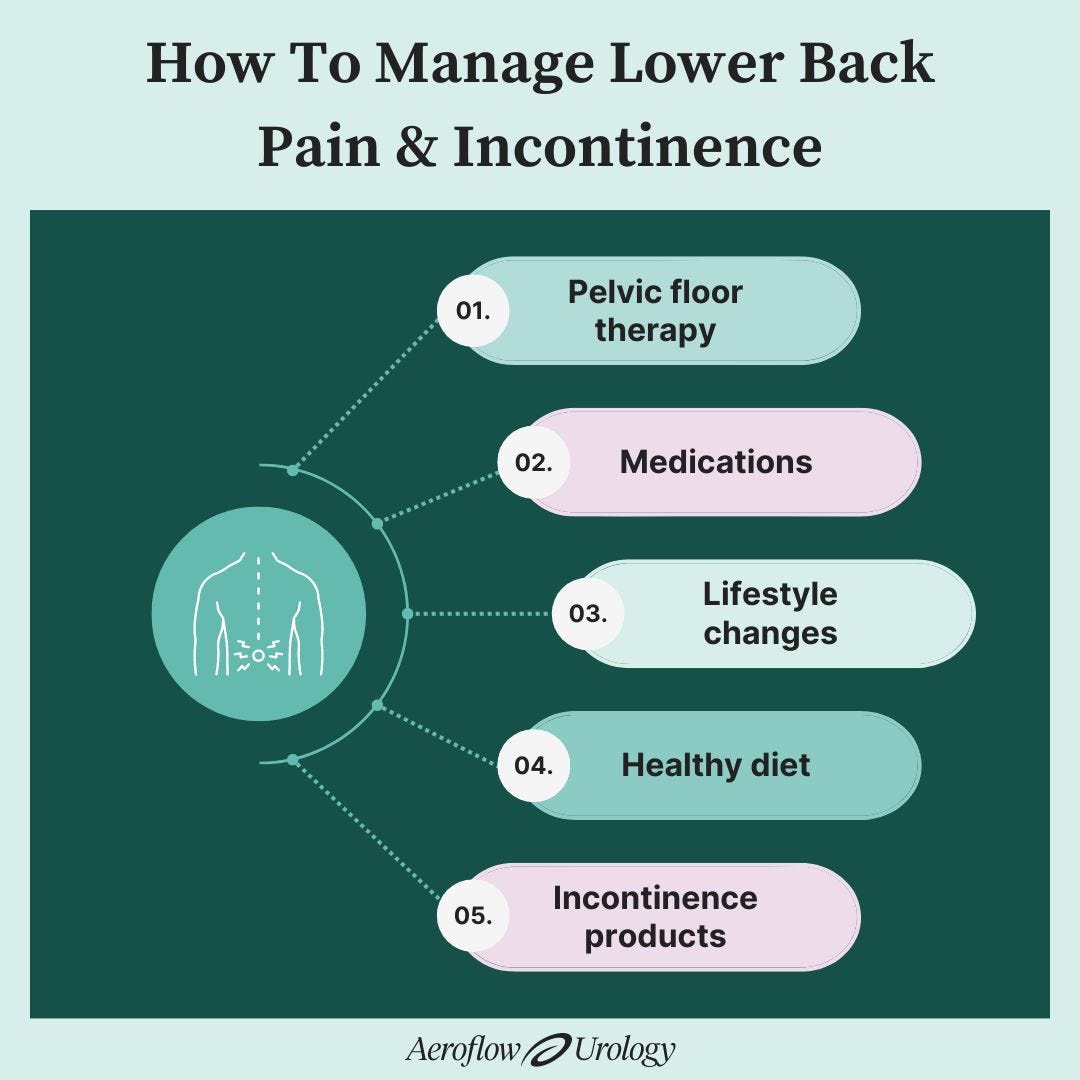
How to Manage Lower Back Pain & Incontinence
If you’re experiencing back pain, incontinence, or both, you can speak with a healthcare professional about your treatment options. They may be able to rule out any serious conditions contributing to the issues, and they can put together a proper treatment plan.
In some cases, incontinence can be treated, but other times can only be managed. Here are some ways to manage your incontinence and lower back pain.
1. Try Pelvic Floor or Physical Therapy
Physical and pelvic floor therapies may help relieve pain and strengthen your pelvic floor muscles over time. Kegel exercises are a common form of pelvic floor exercise, but other options exist for women and men.
2. Use Medication
Generally, medications can assist with back pain and urinary issues. However, if you’d like to steer away from medicine, a back brace or postpartum compression garment are all-natural solutions for relieving pain.
3. Adjust Your Lifestyle
Lifestyle changes may be beneficial for assisting with both back pain and incontinence symptoms. Try to become more active, including at least 30 minutes of moderate exercise three to five times per week. Try swimming, riding a bike, or walking to get yourself up and moving.
4. Eat a Healthy Diet
A healthy diet relieves pressure on your digestive tract. Bladder irritants, such as caffeine, sugar, spicy foods, and alcohol can increase incontinence symptoms. Try adding more water, fruits, vegetables, and whole grains to your diet to relieve constipation and pressure on the bladder. The added nutrition may help with your low back pain as well.
5. Use Incontinence Products
If you have an underlying condition causing incontinence, Aeroflow Urology can provide you with free incontinence products if you qualify.
No one has the time to deal with insurance companies or prescriptions from a healthcare provider. That’s why we do it for you! We’ll work directly with your Medicaid provider to ensure you receive the maximum benefits available. We’ll even ship your supplies directly to your door each month in discreet unmarked packaging, at no cost.
To see if you qualify for incontinence supplies covered through your insurance, follow these easy steps!
1. Fill out our Eligibility Form.
2. If you qualify, one of our Continence Care Specialists will reach out to you and help you find the perfect incontinence supplies for your lifestyle, whether it's adult briefs, catheters, or something else.
3. After choosing your supplies, they will be shipped directly to your door. We'll send a text or email reminder when it's time to re-supply so you'll never run out of incontinence supplies again!
StackPath. (n.d.). Handsdownbetter.org. Retrieved March 29, 2022, from https://handsdownbetter.org/health-and-wellness/back-pain-facts-and-statistics/#:~:text=In%20fact%2C%20about%2031%20million
Shiel, W. C. (2020, August 7). Cauda Equina Syndrome. MedicineNet; MedicineNet. https://www.medicinenet.com/cauda_equina_syndrome/article.htm#cauda_equina_syndrome_facts
Back Pain and Incontinence: Symptoms, Causes, and Treatment. (2017, February 22). Healthline. https://www.healthline.com/health/overactive-bladder/back-pain-and-incontinence#causes-and-risk-factors
Eidelson, S. G. (2014, February 13). Spinal Disorders May Cause Neurogenic Bladder Disorder or Dysfunction. Spineuniverse.com; SPU. https://www.spineuniverse.com/conditions/spinal-disorders-may-cause-neurogenic-bladder-disorder-or-dysfunction
Bush, H. M., Pagorek, S., Kuperstein, J., Guo, J., Ballert, K. N., & Crofford, L. J. (2013). The Association of Chronic Back Pain and Stress Urinary Incontinence. Journal of Women’s Health Physical Therapy, 37(1), 11–18. https://doi.org/10.1097/jwh.0b013e31828c1ab3
UpToDate. (n.d.). Www.uptodate.com. https://www.uptodate.com/contents/evaluation-of-females-with-urinary-incontinence
Co-Author & Editor: Marlee Septak
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.