From the excitement of meeting their child to dealing with morning sickness, pregnant women have a lot to look forward to and a lot of obstacles to face.
What you may not expect during your pregnancy is a loss of bladder control, and while it happens to many women, it’s not normal. Read this post to find out why you’re experiencing urinary leakage and what you can do to help prevent or manage symptoms.
What is Urinary Incontinence?
Urinary incontinence during pregnancy happens to more than one-third of women and is defined as a loss of bladder control leading to the involuntary loss of urine. You may experience different types of urinary incontinence throughout your pregnancy, including:
Stress urinary incontinence (SUI). SUI is the most common type of urinary incontinence experienced during pregnancy and usually occurs during your second and third trimesters. The main symptom of SUI is urine leakage.
This occurs when extra pressure is applied to your abdomen and pelvic muscles—something a growing baby is constantly doing inside of you. You may experience an involuntary loss of urine when you bend over, cough, sneeze, laugh, exercise, or lift heavy objects due to extra pressure placed on your bladder.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
Overactive bladder (OAB). OAB is another common type of incontinence you may experience during pregnancy because your baby’s head puts pressure on your bladder and pelvic floor muscles. With OAB, you may urinate more than normal, feel like you need to void often, and possibly leak urine.
While it’s not a type of incontinence, urinary tract infections (UTIs) are also commonly experienced during pregnancy. UTIs can occur for a couple of reasons: The hormones in your urine alter your urinary tract which can lead to infection, urine retention (not being able to empty your bladder completely), and vesicoureteral reflux (pee is pushed back into the kidneys) can all cause UTIs more easily during pregnancy.
Why Am I Experiencing Incontinence During Pregnancy?
There are a couple of reasons why you may be having bladder control problems while pregnant:
- Your baby. Your baby changes the size of your uterus and how it’s positioned in your body. Your bladder is located underneath your uterus and usually has space to hold a typical amount of urine. Healthy bladders can hold up to two cups of urine daily and four cups while you sleep. But, when you have a baby growing in your uterus, it puts pressure on your bladder, leaving less space for urine, which can be why you experience OAB or SUI. The pressure from a baby can also weaken your pelvic floor muscles and bladder sphincter, causing leakage.


2. Hormones. Hormonal changes, such as progesterone released in your body during pregnancy, affect how well you control your bladder and urethra, leading to leakage.
3. Body fluid. The frequency of urination also occurs during pregnancy because your body fluid increases by 50% while you’re pregnant.
How Long Does Incontinence Last After Pregnancy?
Developing incontinence after your pregnancy (postpartum incontinence) depends on what happened during your pregnancy and delivery.
As your body gets ready to give birth, it changes. On top of experiencing weight gain, your hips loosen, and your cervix, bones, pelvic floor muscles, and pelvic ligaments begin to stretch. This happens in your body so your baby is more comfortable during its growing period and during delivery. All of these changes can lead to postpartum incontinence, depending on how much your body is affected.


Incontinence usually improves after delivery, although it does take time. When you give birth, there are a couple of things that can increase the likelihood that you’ll experience incontinence afterward:
- If your baby is very large, it can affect how much your vaginal canal and vaginal opening stretch, which can, in turn, affect your bladder control.
- If you have an episiotomy (a procedure during which healthcare providers cut your pelvic floor muscle to help the baby come out more easily), you may have much weaker pelvic floor muscles and experience incontinence.
- If you are in labor that lasts for a long time, pelvic nerve damage may occur and lead to incontinence.
- If you have a vaginal delivery, your healthcare providers may use forceps to help the baby out of the vaginal canal. However, this can sometimes damage the sphincter and pelvic floor muscles, causing incontinence. Compared to a cesarean (a procedure where a healthcare provider makes incisions into your abdomen and pulls the baby out through the opening), women who have vaginal deliveries experience incontinence more frequently.
- If you experience a loss of pelvic muscle strength during pregnancy or birth, you may have a pelvic organ prolapse (cystocele) where your organ falls out of its original position, leading to incontinence.


After delivering a baby, your body continues to experience hormonal changes that affect your bladder. Your uterus will begin to go back to its standard size after birth, which can put extra pressure on your bladder, causing incontinence symptoms even after delivery.
It can take anywhere from six to 12 months for your body-including your pelvic floor muscles- to completely recover and heal after giving birth. If you’re breastfeeding or lactating, your normal hormones will continue to be suppressed which can lead to delayed pelvic healing.
How Can I Prevent Incontinence?
Incontinence during pregnancy is common, but it’s not supposed to happen. Use these tips to try and prevent stress incontinence and overactive bladder while you’re going through pregnancy:
- Do Kegel exercises. Kegel exercises, also known as pelvic floor muscle exercises, help you strengthen your pelvic floor. Your pelvic floor muscles increase by more than 200% in preparation for delivery (whether vaginal delivery or Cesarean occurs). Training those muscles to go back to a stable state is key to optimizing pelvic healing postpartum. Yoga stretches and sitting exercises are also great for postpartum incontinence. To perform sitting exercises with your baby, put an exercise ball between your hips and roll your hips to engage your core and pelvic muscles.
- Use a vaginal pessary. A vaginal pessary is a silicone ring that goes into your vagina and may help prevent urinary leakage. Speak with your healthcare provider about getting a vaginal pessary.
- Make lifestyle changes. There are a few ways you can adjust your lifestyle to help manage or prevent incontinence. These include:
- Maintain healthy body weight. Women who are obese experience SUI more frequently than those who are not obese. Weight gain is expected and normal during pregnancy, but the more weight you maintain after pregnancy, the more pressure is put on your bladder.
- Eat a healthy diet. Incorporating fiber into your diet can help ensure that you avoid constipation which can help decrease the likelihood of incontinence.
- Avoid bladder irritants. Certain spicy foods, caffeine, alcohol, carbonated drinks, and certain teas may make your bladder irritated and increase incontinence symptoms.
- Avoid smoking. Smoking can cause incontinence due to chronic coughing and bladder irritation.
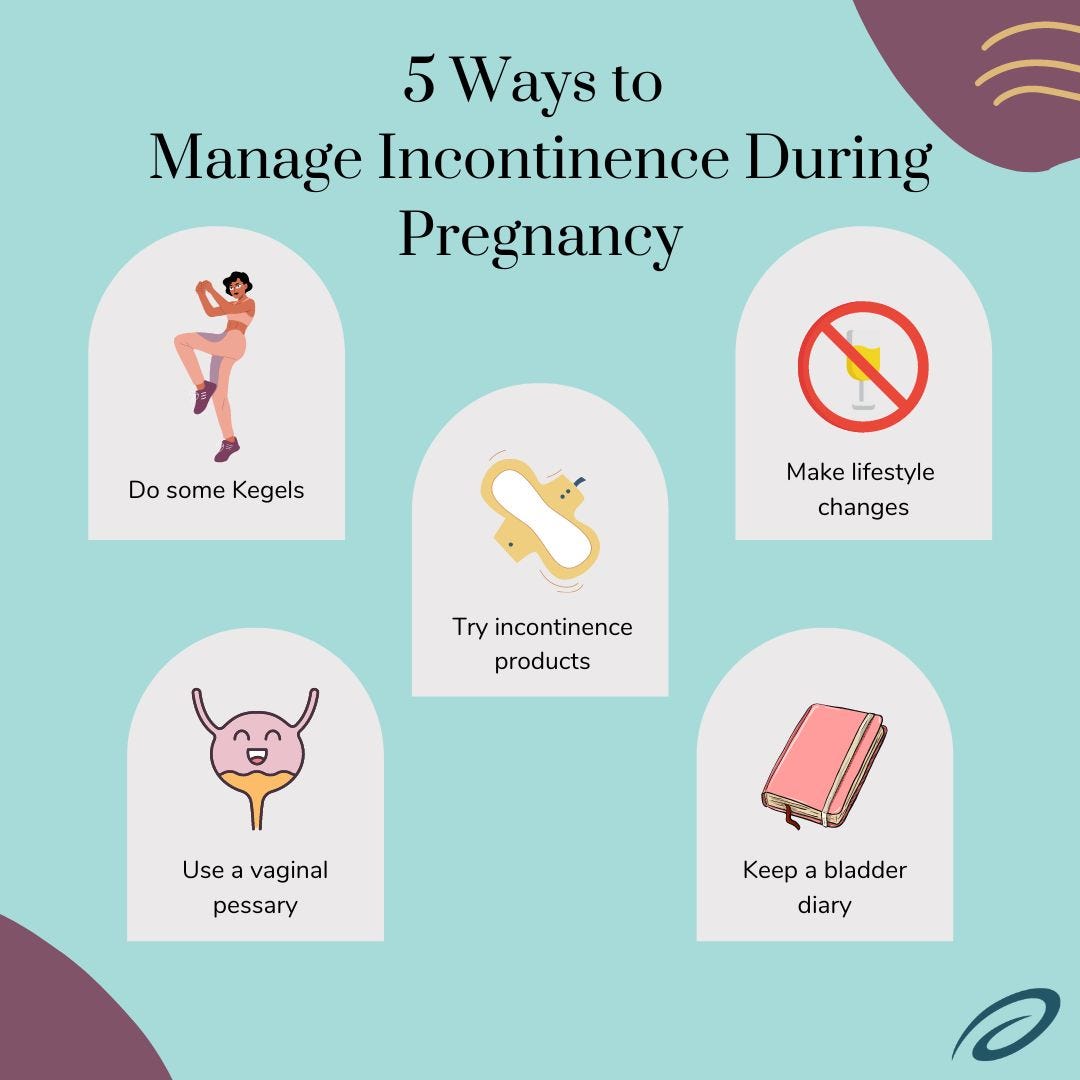
4. Keep a bladder diary. If you can keep track of your leakage and trips to the bathroom, you may be able to train your bladder to be able to hold urine for a longer period of time or determine what is causing your leakage. This is called timed voiding or bladder training.
5. Use incontinence products. If you’re having trouble managing your incontinence symptoms, adult briefs, bladder pads, or Poise pads might be a good option. They are ultra-absorbent and can help manage your leakage.
You should always speak with a healthcare professional, such as your obstetrician, or OBGYN (gynecologist), about preventing incontinence and additional treatment options.
For Postpartum Incontinence
It's important that you take time for yourself after delivery. Self-care is incredibly important and you can't give to others unless you are giving to yourself. Without taking care of yourself postpartum, your pelvic floor muscles may never go back to normal, but it's never too late to retrain those muscles. The sooner you repair the muscles, the less time you have to spend managing incontinence. If you feel you can't take care of yourself and your baby, you can try to do yoga or exercise ball workouts while your new baby sleeps or has tummy time.
How Aeroflow Urology Can Help
If you’re experiencing incontinence after your delivery, Aeroflow Urology may be able to help.
We know that managing incontinence symptoms can be stressful; Making trips to the store, finding out you chose the wrong incontinence product, and spending money on costly incontinence supplies can all take a toll.
Let us help you get incontinence supplies, such as adult briefs, bladder pads, or Poise pads, free through insurance so you can take time to recover after delivery and spend time with your new baby!
Watch the video below to see how Aeroflow Urology can help.
How It Works
The process is simple. Follow these steps to see if you’re eligible to receive supplies through Aeroflow Urology and your insurance plan.
Step 1. Fill out our qualify form.
It's easy and takes under five minutes! Just have your insurance card ready.


Step 2. Once you’ve submitted your information, one of our Continence Care Specialists will reach out and help you fill out all the necessary paperwork.


Step 3. Once approved, you’ll be given a curated shopping list to choose your products from. If you aren’t sure which products will work best for you, don’t worry. Our Continence Care Specialists know everything about our products and will help you find the perfect fit.
Step 4. After choosing your supplies, they’ll be shipped directly to your door in discreet packaging.
We’ll also send you monthly text or email reminders to let you know when you need to resupply so you won’t have to worry about being without incontinence supplies in the future.
References:
Tips to prevent involuntary urine leakage (incontinence) during and after pregnancy | Women’s Health | Your Pregnancy Matters | UT Southwestern Medical Center. (n.d.). Utswmed.org. Retrieved April 6, 2022, from https://utswmed.org/medblog/leakage-incontinence-during-after-pregnancy/#:~:text=More%20than%20a%20third%20of
Pregnancy Incontinence - Pregnancy Pelvic Floor Exercises - Poise. (n.d.). www.poise.com.au. Retrieved April 6, 2022, from https://www.poise.com.au/female-incontinence/pregnancy
Sangsawang, B., & Sangsawang, N. (2013). Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment. International Urogynecology Journal, 24(6), 901–912. https://doi.org/10.1007/s00192-013-2061-7
What if I Get a Urinary Tract Infection (UTI) While I’m Pregnant? (n.d.). WebMD. Retrieved April 6, 2022, from https://www.webmd.com/women/guide/pregnancy-urinary-tract-infection#:~:text=When%20you
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.