The cycle of managing nighttime accidents can feel never-ending at times; changing wet pajamas, washing soiled sheets, and getting your child back to sleep all contribute to the challenges of bedwetting.
If you’re looking for a solution for your loved one, a bedwetting alarm may be helpful, but it’s important to understand the purpose of these alarms, as well as which types of children may benefit from them.
In this article, we’ll share all you need to know about bed-wetting alarms and help you determine if your child is ready to use one.
What Is Nocturnal Enuresis?
Chronic bedwetting is a type of urinary incontinence known as nocturnal enuresis (NE). NE is described as an involuntary loss of urine while sleeping.
Those with NE are typically older than 5 years old and wet the bed at least 2 times per week for 3 months or longer. NE can happen to children, teens, adults, and seniors, but it is very common among children. In fact, it’s the most common problem spoken about among parents of children with a form of urinary incontinence (UI).
Check Your Child's Eligibility
In Less Than 2 Minutes
From diapers to pull-ups, discover the continence care essentials covered by your insurance.
People who experience NE range from children to adults. Studies show:
- 20% of 5-year-olds have NE.
- 15% of 7-year-olds have NE.
- 10% of 10-year-olds have NE.
- 2% of adolescents have NE.
- .5% to 1% of adults have NE.
Studies also show that NE is more common in boys than girls.
Causes of NE
Genetics: Children with NE usually inherit the condition from their parents; Studies show that:
- 44% of kids diagnosed with NE have 1 parent who also experienced bedwetting as a child.
- 77% of children with NE have 2 parents who experienced it when they were children.
Psychological factors: Psychological factors, such as post-traumatic stress disorder (PTSD), stress, fear, sexual abuse, and more, are now considered to be causes of NE in children.
Lifestyle choices: Things like diet and bathroom habits can also contribute to NE.
Other conditions: Certain conditions can lead to NE in children. These include:
- Constipation
- Urinary tract infections (UTIs).
- Cystitis
- Diabetes insipidus.
- Small bladder capacity.
- Overactive bladder (OAB).
- Decreased levels of the anti-diuretic hormone (ADH).
- Urethral obstructions.
- Certain neurological conditions (autism, ADHD, etc.).
- Certain medical conditions (Spina bifida, etc.).
- Sleep disorders.


What Is a Bedwetting Alarm?
A bedwetting alarm, also known as an enuresis alarm, was designed to help children stop bedwetting.
The alarm unit is activated when your child begins to leak urine onto the alarm’s moisture sensor. When the device senses moisture, the alarm sounds are activated with the goal of waking your child from sleep and stopping them from having an accident.
These bedwetting enuresis alarms were created in 1938 by Hobart and Willie Mowrer. The first prototype included a bed pad or mat that contained an electrical circuit. When the child’s urine leaked onto the circuit, a bell would ring.
Today, there are different types of bedwetting alarm systems that may be able to help your child overcome NE, depending on their unique needs and conditions.
Current bedwetting alarms operate by using a moisture sensor that is placed in your child’s pajamas or around their arm that triggers an alarm sound or buzzer when the first drop of urine is leaked onto the sensor. The alarms are made to wake your child up so they can use the bathroom rather than pee in the bed. Certain alarms are also designed loudly enough to wake the parent so they can help the child go to the bathroom.
While most alarms operate similarly (volume control, moisture sensor, wearable alarms), certain things do differ and prices can range from $50 to over $150.
- Wired alarm: A wire runs from the system’s moisture sensor to the alarm.
This alarm is attached to your child’s clothing near their shoulder area with an armband and the moisture sensor goes inside their pajamas near the underpants. When the system senses moisture, a buzzer or sound will go off to wake your child.
- Wireless alarm: These alarms are silent and rather than making a loud sound when they’re activated by moisture, they vibrate. Wireless bed-wetting alarms are sometimes preferred for adolescents, teens, and adults.
- Bedside bedwetting alarm: An alarm that sits near the bed or on the nightstand.
Do Bedwetting Alarms Work?
Do bedwetting alarms work for bladder control at night?
While the success rate of a bed-wetting alarm will be dependent upon your child’s unique needs, studies show that they do help stop overnight voiding.
In one study, over 76% of children with NE who used a bed-wetting alarm had 14 dry nights consecutively while only 2% of those who didn’t use an alarm had the same number of dry nights.
Healthcare providers may recommend a bed-wetting alarm for your child as an effective and safe treatment to maintain dryness throughout the night. Children usually need to use the alarm for around 3 months to see results.
If your child manages other conditions, such as PTSD, is a deep sleeper, or has a special need (autism, Down syndrome, etc.), they may need extra help while using the alarm system or it may take longer to see results.
What to Consider Before Buying a Bedwetting Alarm
Before purchasing an alarm system for your child, ask yourself these 4 questions to determine if they’ll have success with the alarm system.
1. Do you know the cause of your child’s bedwetting?
If your loved one has any correlating conditions that may be the cause of their NE, such as a special need, constipation, UTIs, sleep disorders, etc., a bed-wetting alarm may not work for them. It’s best to speak to your child’s pediatric healthcare provider before purchasing a bed-wetting alarm to determine the cause of their NE.
2. Is your child ready?
It’s important that your loved one is ready and able to use a bed-wetting alarm system. Not only will this will result in a higher chance of success, but it will also lessen the fear or frustration they may experience when being woken up in the middle of the night by an unfamiliar sound. Speak with your loved one about using the alarm and ensure they’re ready and willing.
3. Do you know what type of alarm will work for your child?
Each child with NE has unique needs and conditions, so it’s important to choose an alarm that’s suitable for them.


Is your child older and would prefer a silent, vibrating alarm? Does your child have a sleep disorder that would prevent them from hearing the alarm? Answer these types of questions before deciding which system to purchase, and speak with your child’s healthcare provider if needed.
4. Are you prepared to help?
Helping your child eliminate symptoms of NE can be a lengthy process in certain cases, so before you begin, ask yourself if you’re prepared to be patient, understanding, and, obviously, awake more often at night to help your child with whatever they may need.
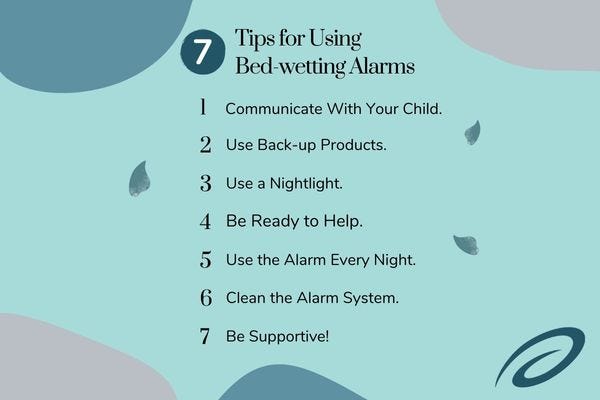
Tips for Beginners
Helping your loved one overcome bedwetting can be a long process and experimenting with a bed-wetting alarm may be just one piece of the puzzle. Remember these tips when using your child’s alarm for the first time.
1. Communicate With Your Child.
Make sure your child knows you’re using the alarm as a way to help them sleep through the night and not as a form of punishment or a source of embarrassment. You can have them help set the alarm up and practice using it a couple of times before sending them off to bed so the sound isn’t too frightening.
2. Use Back-up Products.
Pediatric diapers and pull-ups with overnight absorbency can be helpful if your child’s bed is wet or if you are not seeing success with the bed-wetting alarm. Depending on your child’s insurance, the state they live in, and their unique condition, they may qualify for free diapers or pull-ups. Find out in under 5 minutes.
3. Use a Nightlight.
When your child awakes after their alarm sounds, they’ll need to find the bathroom to urinate. It may be helpful to have a flashlight or nightlight in their room so they can navigate their way to your bedroom or to the toilet.
4. Be Ready to Help!
Children who first start using bed-wetting alarms might not wake up the first couple of times the alarm goes off, and if they do, they may be frightened. Be prepared to wake up and help them shut the alarm off, use the bathroom, or change the bedding if they do have an accident.
5. Use the Alarm Every Night.
You should aim to use the bed-wetting alarm each night for 3-4 weeks or longer until your child experiences dry nights. If they continue to be unsuccessful, speak with their pediatrician.
6. Clean the Alarm System.
Keep the bed-wetting alarm system sanitary for your child to use by cleaning it per your system’s specific instructions.
7. Be Supportive!
Retraining your bladder is a challenging task! Your child may feel discouraged if they don’t see progress within the first couple of nights or weeks, so be encouraging with kind, supportive words. You can also use a reward system if your child responds to rewards.
Bedwetting. (n.d.). Www.aacap.org. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Bedwetting-018.aspx
Gomez Rincon, M., Leslie, S. W., & Lotfollahzadeh, S. (2020). Nocturnal Enuresis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK545181/
Centre (UK), N. C. G. (2010). Enuresis Alarms in the management of bedwetting. In www.ncbi.nlm.nih.gov. Royal College of Physicians (UK). https://www.ncbi.nlm.nih.gov/books/NBK62711/
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.