Postpartum Incontinence:
Reclaim Your Confidence After Childbirth
You’re not alone in managing postpartum incontinence. We’re here to help you find support and get free bladder control supplies.
Motherhood should be about bonding and joy, not silent struggles with postpartum incontinence.
Our survey of over 1,000 new moms revealed that nearly 90% experience this common but often unacknowledged challenge, and fewer than 15% of new mothers get the postpartum resources they need from their healthcare provider.
We're here to change that and support you.
What Is Postpartum Incontinence?
Childbirth is an incredible feat, but it undeniably transforms your body. During pregnancy, organs shift, and increased pressure is placed on the bladder and pelvic floor muscles. This can lead to weakening over time, compounded by the stretching that occurs as the baby passes through the birth canal.
While the initial recovery period is often cited as six weeks, the body can take significantly longer – up to a year – to fully heal. Hormonal fluctuations and the uterus returning to its normal size further contribute to bladder instability.


There are two main types of postpartum incontinence you can experience.
-
Stress Incontinence: This occurs when physical activities such as coughing, sneezing, laughing, or exercising put pressure on the bladder, causing urine leakage.
-
Urge Incontinence: This is characterized by a sudden, intense urge to urinate, followed by an involuntary loss of urine.
“The first thing that we need to talk about is the acknowledgement that this is a very common concern that is actually happening, versus saying, ‘Oh, it’s just normal,’” says Aleece Fosnight, MSPAS, PA-C, CSC-S, CSE, NCMP, IF, HAES. “Most of the time, people also think that it’s normal, then, for them to leak urine on themselves, or even to leak stool.”
Postpartum incontinence can be temporary, but for some individuals, it persists for months or even longer if not properly managed. It can significantly impact a woman’s daily life, mental health, and overall quality of life.
Postpartum Incontinence Survey Data
Aeroflow Urology recently conducted a comprehensive survey of over 1,000 new mothers to understand their experiences with postpartum incontinence, a common issue following childbirth.
Motherhood should be about bonding and joy, not silent struggles with postpartum incontinence.
Our survey of over 1,000 new moms revealed that nearly 90% experience this common but often unacknowledged challenge, and fewer than 15% of new mothers get the postpartum resources they need from their healthcare provider.
We're here to change that and support you.
Check your coverage for 100% free incontinence products now!
Check your coverage for 100% free incontinence products now!
"As a mom of three, postpartum incontinence was something I never expected to impact my motherhood journey as much as it did. It never really was a problem - until this third and last postpartum journey. It wasn’t just about leaking when I laughed or sneezed—it was the constant worry, the extra planning, and the feeling that my body wasn’t entirely mine anymore. No one really prepares you for that. I wish there was more open conversation around postpartum incontinence, along with real support—whether that’s access to pelvic floor therapy, better postpartum education, or just knowing you’re not alone. Motherhood is already an emotional rollercoaster, and no mom should have to navigate this silently or feel embarrassed by something so common."
-Alexis K.
"As a mom of three, postpartum incontinence was an unexpected challenge that impacted my daily life and confidence. Simple activities like laughing, sneezing, or running after my kids became moments of anxiety. It’s something so many mothers experience, yet it’s rarely talked about openly. I wish there was more accessible education and proactive support, from doctors normalizing the conversation to brands providing better resources and products tailored to real postpartum recovery. Moms shouldn’t have to just ‘deal with it’—we deserve solutions that help us feel strong and supported in our motherhood journey."
-Isabella M.
Impact of Postpartum Incontinence
Mental Health
Incontinence can take a significant toll on the emotional and mental health of any individual managing the condition, but its impact on new parents can be especially devastating.
After giving birth, individuals may develop perinatal depression and 20% experience anxiety in the early postpartum period. Our survey found that 71% of mothers felt anxious, stressed, and self-conscious because of their postpartum incontinence. The added burden of managing anxiety and depression, compounded by the mental health challenges of incontinence, places a severe strain on new parents.
Prioritizing your mental health is crucial when dealing with postpartum incontinence. Connecting with a mental health professional can provide invaluable support during this time.
While professional guidance is highly beneficial, remember that your support network extends beyond therapists. Leaning on close friends and family can also make a significant difference in navigating this challenging period.
Mental Health &
Postpartum Incontinence
27% of mothers feel self-conscious
23.6% feel stressed
21.03% feel anxious
13% feel depressed
Daily Routines
New mothers often feel confined to their homes to care for their babies, and postpartum leakage further disrupts their daily activities. Our study revealed that bladder leaks hinder the daily routines of 3 out of 4 mothers. Additionally, 76% of mothers reported experiencing bladder leakage during everyday tasks, such as sneezing, laughing, and doing chores.
“After having my four children, I started experiencing incontinence issues. It only got worse as the years passed. Coughing, sneezing, laughing, yelling, jumping all affect me on a daily basis.”
-Felicia L.
The Postpartum Healthcare Gap
80% of mothers in our study felt their healthcare provider could have done more to educate them about postpartum incontinence, and this falls in line with what seems to be a prevalent trend among all adults with incontinence, not just new parents with postpartum incontinence.
Many adults with incontinence feel they receive low-quality care from their providers when it comes to incontinence management, and that could partly be because healthcare providers aren’t trained in incontinence management. In a paper by the International Continence Society, it was noted that the lack of continence training among healthcare professionals is a world-wide issue.
“It’s society’s responsibility to focus on postpartum incontinence,” says Lopa Pandya, MD, MS, FACOG. “Women’s health in general, and taking care of people who have babies and who deal with issues after having children is poorly funded in this country.”
Among the mothers surveyed in our study, nearly 90% wish they had received more postpartum incontinence resources from their provider. In order to provide proper resources, the healthcare industry must become more aware of the need that exists.
“Healthcare providers need to acknowledge that this is happening, that this is life-disrupting, that this is something that could occur,” says Pandya. She says simple acknowledgement can go a long way with those experiencing postpartum incontinence, and that knowing that there’s a chance that symptoms can get better can be very comforting.


Postpartum Incontinence Resources for Mothers
If you’re a mother experiencing postpartum incontinence, Aeroflow Urology is here to help and support you.
Tips for Postpartum Incontinence Management
If you’re experiencing postpartum incontinence, use these tips to manage your symptoms.
- Incontinence supplies. Regain your confidence and comfort with bladder control supplies designed to manage postpartum incontinence. From discreet bladder control pads to pull-ons and overnight briefs, there's a solution for every level of leakage. Even better, these products may be covered by your insurance! Check your coverage with Aeroflow Urology's simple Eligibility Form and let us handle the rest, so you can focus on what matters most – your new baby.
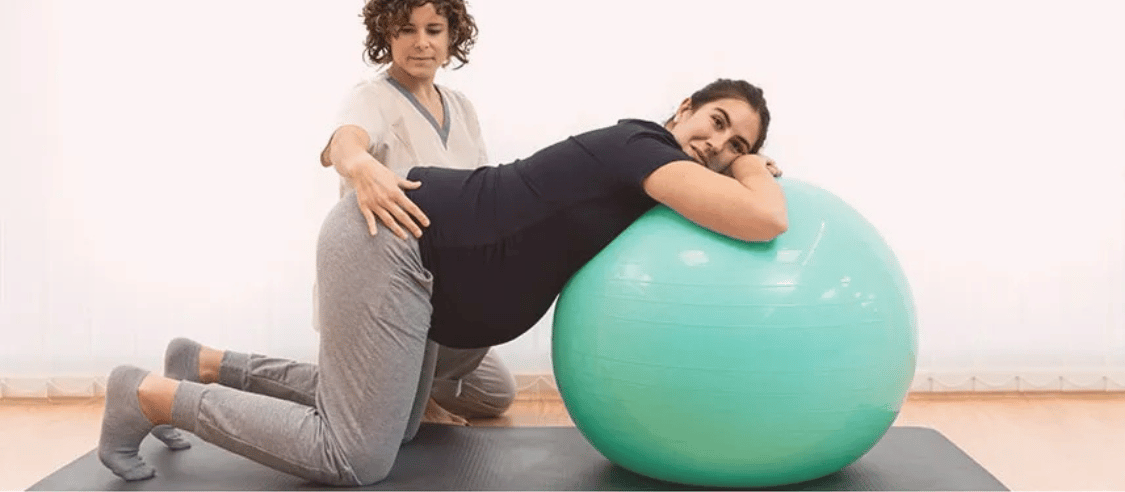
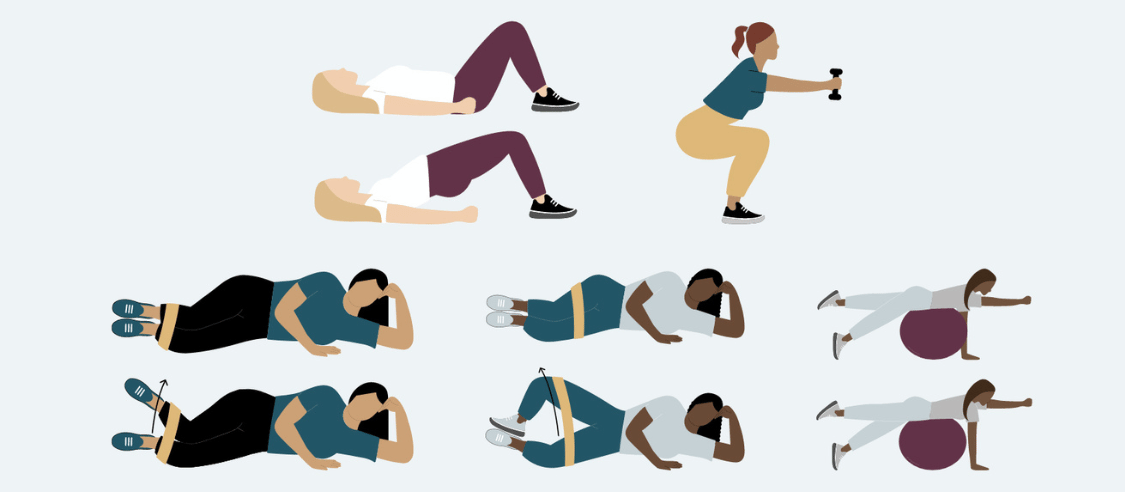
- Kegel exercises. Starting off with simple Kegel exercises can be very helpful in reducing symptoms of leakage. If you’re unsure of how to perform these types of pelvic floor exercises, you can use online tutorial videos as guides. Pandya recommends referencing videos from licensed pelvic floor physical therapists. “If you start doing these exercises at home, it can definitely be beneficial to your symptoms,” she says.
- Diet modifications. Certain foods, like spicy foods, alcohol, caffeine, and carbonated drinks can irritate your bladder. Avoid these items and instead, nourish your body with fiber-rich fruits and vegetables and whole grains.
- Hydration. Drink plenty of water throughout the day. Aim for eight glasses to support bladder health and prevent dehydration.
- Education. “I do think that there’s a lot of information out there to give to patients, so acknowledgement and education– even if the provider themself is not doing the counseling– just getting information out there can be helpful,” says Pandya. Ask your healthcare provider for information on postpartum incontinence before, during, and after childbirth.
- Bladder training. Retrain your bladder by going to the bathroom every 30-60 minutes initially, then gradually extending the time. Pre-activity emptying can also help reduce incontinence.
- Pelvic floor therapy. Pandya suggests getting a referral to a pelvic floor physical therapist from your healthcare provider. A pelvic floor physical therapist can help you strengthen your pelvic floor muscles and reduce symptoms of incontinence.
Postpartum Incontinence Articles
Take control of your postpartum recovery. Our blog offers valuable insights and techniques to help you manage incontinence.
Postpartum Incontinence Videos
Discover practical strategies to reduce incontinence symptoms and regain your confidence. Watch our insightful videos from our Medical Advisors or head over to Aeroflow Urology’s YouTube channel for more incontinence information.
Resources for Providers
As a healthcare provider, you play a key role in helping your patients navigate postpartum incontinence. Explore these resources to enhance your care and support.
Helping Your Patients with Postpartum Incontinence
Support your patients' recovery by connecting them with Aeroflow Urology. We provide free bladder control products through Medicaid and private insurance if your patient qualifies, making it easier for new parents to manage incontinence and focus on their well-being.
Easy Referral Process:
- Diagnose & prescribe: If your patient has postpartum incontinence and is enrolled in a qualifying insurance plan, simply download our Patient Order Form to prescribe incontinence supplies.
- Connect with Aeroflow Urology: Have your patient submit their insurance information through our Eligibility Form, and we'll quickly determine their coverage.
Check Your Eligibility
Discover the incontinence supplies available through your insurance plan.


References:
National Institute of Mental Health. (2023). Perinatal Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/perinatal-depression
Nakić Radoš, S. (2018). Anxiety during pregnancy and postpartum: Course, predictors and comorbidity with postpartum depression. Acta Clinica Croatica, 57(1), 39–51. https://doi.org/10.20471/acc.2018.57.01.05
Percival, J., Abbott, K., Allain, T., Bradley, R., Cramp, F., Donovan, J., McCabe, C., Neubauer, K., Redwood, S., & Cotterill, N. (2023). Hospital practitioner views on the benefits of continence education and best ways to provide training. Nursing Open, 10(5), 3305–3313. https://doi.org/10.1002/nop2.1582
Gordon, B. (n.d.). Continence Promotion, Education & Primary Prevention Continence Foundation of Australia 2. PHYSICIANS (FAMILY PHYSICIANS/ GENE- RAL PRACTITIONERS/PRIMARY CARE PHYSICIANS) 3. NURSING PROFESSIONALS 4. PHYSIOTHERAPY AND OTHER ALLIED HEALTH PROFESSIONALS 5. I. https://www.ics.org/Publications/ICI_4/files-book/comite-21.pdf