Medicare Coverage & Advocacy Guide
We understand the challenges and frustrations that come with managing incontinence, especially when essential products are not covered by Medicare. Our mission is to support your health and well-being by offering reliable solutions and advocating for better coverage.
Learn about Medicare coverage and join us in our advocacy efforts to ensure that incontinence supplies are recognized as necessary by Medicare for a better quality of life.
What's the Difference Between Medicare & Medicaid?
Insurance plans can be difficult to understand, so let’s break down the main differences between Medicare and Medicaid.
Both are public health insurance programs but differ in costs and service coverage.
Medicare
Medicare is a health insurance program that’s federally run and regulated by the Centers for Medicare and medicaid (CMS).
Am I Covered?
Find Out In Under 2 Minutes
Discover the continence care essentials available through your Medicaid plan.
Who Qualifies for Medicare?
To qualify for Medicare, you usually need to:
- Be 65 or older.
- Be 65 or under with a disability or special need.
- Have end-stage renal disease (permanent kidney failure).
- Unlike Medicaid, Medicare is available for people who fit the above specifications, regardless of their income.
Medicaid
Medicaid is a public healthcare program that’s federally and state run. Because Medicaid is run by individual states, coverage varies widely based on your residency and type of Medicaid plan you are enrolled in.
Medicaid coverage varies by state, so your plan may be a Medicaid-managed care plan or a general Medicaid state plan.
Who Qualifies for Medicaid?
Those who qualify for Medicaid do not need to meet all of the requirements listed under the Medicaid Eligibility Groups list but usually meet a combination of some of the following requirements:
- Have low income.
- Elect for COBRA coverage.
- Are elderly.
- Are institutionalized.
- Children in foster care or guardianship care.
- Receive Supplemental Security Income (SSI).
- Have special needs or disabilities.
Does Medicare Cover Incontinence Supplies?
Unfortunately, Medicare currently does not consider incontinence products medically necessary items, so these types of Medicare plans do not cover incontinence supplies. If you have Medicare, you will most likely have to pay out-of-pocket costs for your necessary incontinence supplies.
Do Medicare Advantage Plans Cover Incontinence Supplies?
Some Medicare Advantage plans may offer over-the-counter (OTC) benefits which can be used to help cover your cost of incontinence supplies. It’s best to check with your Medicare Advantage plan directly to see options you may have available.
Take Action to Advocate for Incontinence Supplies Covered by Medicare
At Aeroflow Urology, we understand how frustrating it can be that Medicare does not cover incontinence products, as they are not deemed medically necessary.
We believe these essential products play a critical role in maintaining your health and quality of life, and that every person should have access to these supplies, without costs attached.
While we continue to advocate for better Medicare coverage, your voice is powerful. If you feel that these products should be covered by Medicare, we encourage you to take action by sending an email to your state representative.
Together, we can make a difference and work towards getting better incontinence supply coverage for everyone.
How to Find Your State Representative
It’s easy to advocate for expanded Medicare coverage. Follow these steps to email your representative.
- Go to the house.gov website to use their state representative locator.
- Enter your zip code to find your representative.
- Use the email template we have below in your email, addressing your representative by name.
- Send your email and help advocate for free incontinence supplies through Medicare!


Ready-to-Use Email Template
Subject: Urgent Request: Advocate for Expanded Medicare Coverage for Incontinence Products
Dear [Your Representative's Name],
I hope this message finds you well. I am writing to you as a concerned constituent in [Your State / District] to draw your attention to a critical issue affecting many individuals with disabilities and incontinence: the lack of Medicare coverage for incontinence products.
As you may know, Medicaid currently provides free incontinence products to those who qualify, helping to alleviate the financial burden and improve the quality of life for countless individuals. However, Medicare, which serves as a vital lifeline for millions of seniors and people with disabilities, does not offer the same coverage. This gap leaves many struggling to afford the essential products they need to maintain their dignity, health, and independence.
Incontinence is a common condition that affects a significant portion of the Medicare population. The inability to access necessary incontinence products can lead to severe physical and emotional consequences, including skin infections, urinary tract infections, and a profound sense of embarrassment and isolation. These outcomes not only diminish the quality of life for affected individuals but also result in higher healthcare costs due to the complications arising from inadequate management of incontinence.
I urge you to advocate for the expansion of Medicare coverage to include incontinence products. By doing so, we can ensure that all individuals with disabilities and incontinence have access to the supplies they need to lead healthy and dignified lives. This change would align Medicare with Medicaid's existing coverage, creating a more equitable healthcare system and addressing the urgent needs of our aging population.
Please consider sponsoring or supporting legislation that addresses this critical issue, or helping Aeroflow Urology to advocate for these legislations. Expanding Medicare coverage for incontinence products is a compassionate and necessary step towards ending diaper need and ensuring that our most vulnerable citizens receive the care and support they deserve.
Thank you for your attention to this important matter. I look forward to your support and action on behalf of those in our community who are struggling with incontinence.
Sincerely,
[Your Full Name]
[Your Address]
[City, State, ZIP Code]
[Your Email Address]
[Your Phone Number]
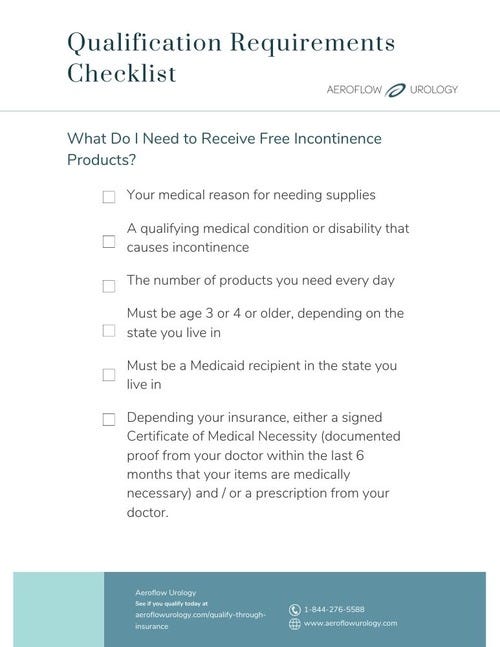
Get Free Incontinence Supplies With Medicaid
If you have Medicare coverage and require incontinence supplies to manage a bladder or bowel control condition, you can try applying for Medicaid so your products are covered. Once your insurance coverage is approved, you can use Aeroflow Urology to receive free incontinence products through your Medicaid coverage.
We offer a wide variety of medical-grade adult diapers, bladder control pads, catheters, underpads, pediatric diapers, pull-ups, and more supplemental items, all through insurance. Our products are suitable for individuals of all ages, from older adults to children (ages 3+). Our absorbent and protective supplies are also suitable for an array of medical conditions.
If you have Medicaid, get started today by filling out our simple Eligibility Form. It takes less than 2 minutes to complete, and our team of Continence Care Specialists will inform you of your coverage in 1-2 business days via email and text.
Disclaimer
*Medicaid coverage varies by state. Submitting your info is not a guarantee of benefit.
Jump To: Top | Eligibility Form