This piece has been medically reviewed by Aleece Fosnight, MPAS, PA-C, CSC-S, CSE, NCMP, IF, Medical Advisor to Aeroflow Urology.
A breast cancer diagnosis is never easy to receive, and managing cancer is a difficult journey. Most people are aware of symptoms during breast cancer treatment and the changes that occur in their bodies after recovering, but one symptom related to breast cancer and cancer treatment that’s being newly researched is urinary incontinence (UI), or the loss of bladder control.
This post will tell you:
- How breast cancer is linked to UI.
- How UI is a symptom of cancer treatments.
- Which types of pelvic floor dysfunction and bladder problems are seen in breast cancer survivors.
- What you can do to manage your UI symptoms to regain your quality of life.
Check Your Eligibility
2 Easy Steps
Discover the continence care essentials available through your Medicaid plan.
UI & Breast Cancer
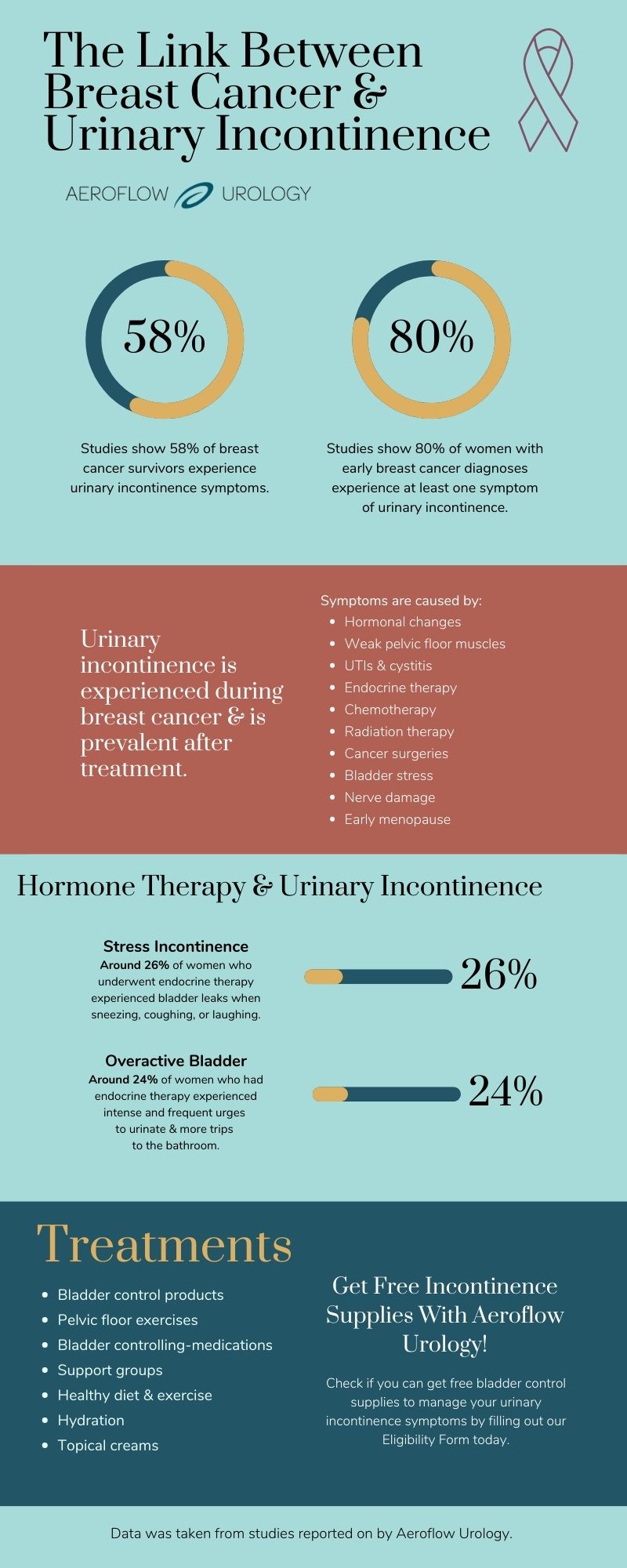
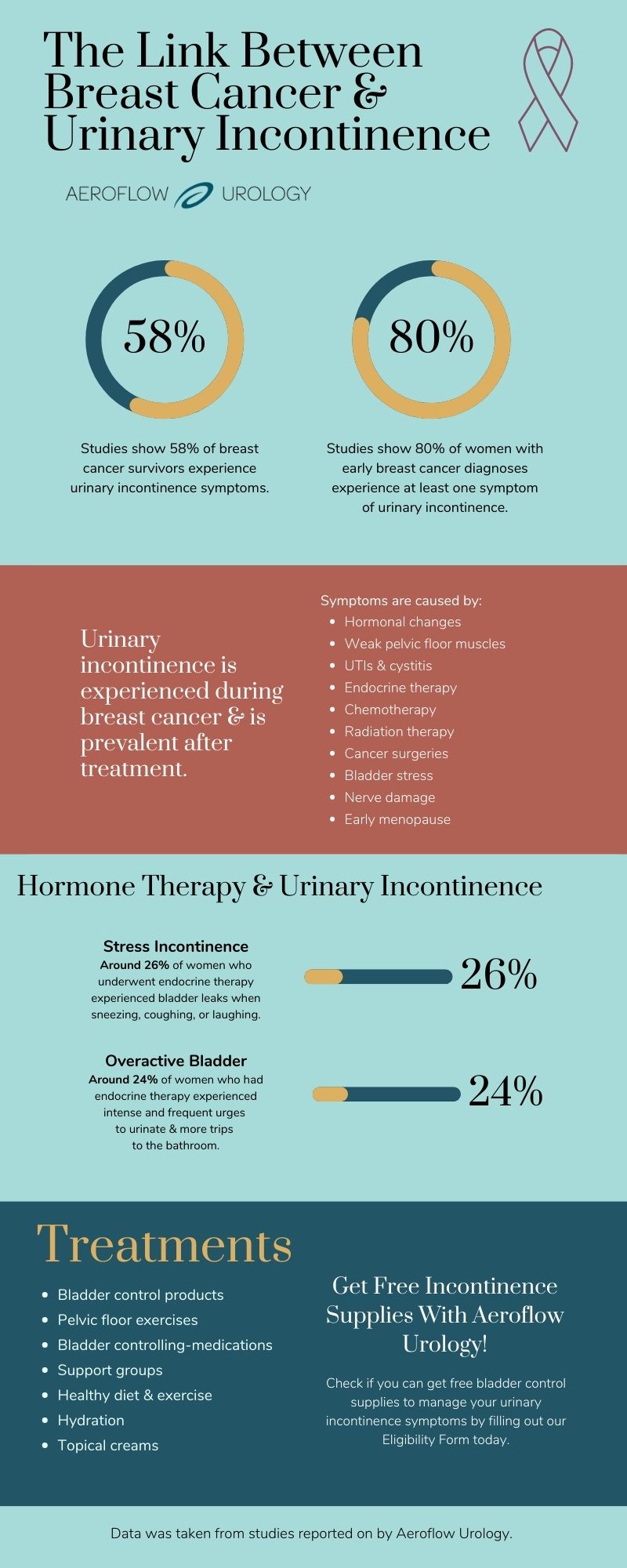
It’s been shown that UI, or the loss of bladder control, is linked to breast cancer diagnoses.
One study showed that bladder leakage was prevalent in women around the age of 54 who were diagnosed with early-stage breast cancer. In addition, the study revealed that women with breast cancer experienced different types of incontinence.
- 80% were bothered by at least 1 UI symptom.
- Around 40% experienced mixed incontinence, a mix of more than 1 type of UI.
- About 29% experienced overactive bladder (OAB) / urge incontinence, or feeling the sudden and frequent urge to pee, resulting in voiding your bladder more than 8 times in 24 hours.
- About 10% experienced stress incontinence, experiencing urine leaks when sneezing, coughing, laughing, lifting heavy objects, or exercising.


Women with breast cancer are also at an increased risk of developing urinary tract infections (UTIs) and cystitis. A study showed that out of 100 women with breast cancer:
- 5% developed UTIs, or an infection of the urinary system in which bacteria enter through the urethra and cause symptoms such as pain when urinating.
- 8% developed cystitis, a type of UTI that causes bladder inflammation.
Breast cancer can also cause hormonal changes that dry the urethra, increasing your chances of developing UI.
While more research is needed to show that UI and urinary system infections are early symptoms of breast cancer, you should speak with your healthcare provider if you’re experiencing these symptoms and have been diagnosed with breast cancer.
UI & Breast Cancer Treatments
The most common genitourinary symptoms experienced by breast cancer survivors are vaginal dryness and hot flashes. Still, it’s also been shown that UI and pelvic floor issues can be side effects of different types of cancer treatments. In fact, up to 58% of breast cancer survivors report experiencing UI symptoms after treatments.
The types of breast cancer treatments resulting in UI symptoms are:
- Endocrine therapy.
- Chemotherapy
- Radiation therapy.
- Mastectomy or lumpectomy.
Endocrine Therapy
Endocrine therapy (also known as hormone therapy) is a treatment for breast cancer that slows or halts the growth of your cancerous tumors. These tumors are sensitive to hormones, such as estrogen, and these hormones can encourage tumor growth.
During endocrine therapy, your healthcare provider will prescribe a pill to be taken orally that will create hormone changes in your body and slow or stop tumor growth. Endocrine therapy usually happens after all other breast cancer treatments are performed, and the type of hormone therapy you receive will depend on whether you are experiencing menopause.
While endocrine therapy is successful, it’s been shown to cause UI symptoms. One study showed that women with breast cancer developed UI symptoms, such as stress incontinence, after undergoing endocrine therapy.
Another study, including women with breast cancer, revealed that after endocrine therapy treatment:
- Almost 50% had UI symptoms.
- About 26% experienced stress incontinence.
- Around 24% experienced OAB.
Chemotherapy
Chemotherapy is a breast cancer treatment that stops the growth of cancer cells by killing them or preventing them from dividing. Chemotherapy consists of taking an oral, injection, or IV of the drugs that will kill or shrink the cancerous cells.
Women with breast cancer who have undergone chemotherapy have reported UI symptoms. This is due to:
- Nerve damage: Chemotherapy can cause nerve damage which weakens pelvic floor muscles or cause bladder leakage.
- Bladder stress: Chemotherapy may cause nausea and vomiting, putting extra stress on your bladder and pelvic floor muscles.
- Hormone changes: With chemotherapy, you may experience hormonal changes that can cause UI symptoms due to vaginal dryness.
- Early or temporary menopause: Regardless of where women receive chemotherapy on their bodies, the treatment will attack cells in the ovaries, causing early-onset or temporary menopause. Menopause can come with symptoms such as vaginal dryness, leading to UI.
Radiation Therapy
Radiation therapy treats breast cancer by sending energy beams through x-rays or gamma rays to a localized area on your body where cancerous cells are growing. Radiation therapy destroys cancer cells and consists of undergoing a series of treatments.
Women undergoing this type of cancer treatment experience fibrosis scarring that may cause UI symptoms and stop blood flow.
Radiation therapy may also damage the nerves that control your bladder (give you continence), resulting in bladder leakage.
Surgeries
Breast cancer surgeries, such as mastectomies or lumpectomies, can also cause UI symptoms in women, such as:
- Constipation: Constipation places extra pressure on your bladder, which may lead to OAB symptoms. Constipation can arise following breast cancer operations due to decreased physical activity or a diet lacking in fiber.
- Weakened pelvic floor muscles: Following surgery, you may move or exercise less and sit more, weakening pelvic floor muscles.
How to Manage UI Symptoms
There are many treatment options for those who have UI symptoms. If you have been diagnosed or have survived breast cancer, you can use these tips to reduce UI symptoms, but you should always speak to your healthcare provider to ensure these treatments don’t interfere with your cancer treatment plan.
1. Pelvic Floor Exercise
Kegel exercises strengthen your pelvic area and lessen UI symptoms like stress incontinence leakage. Kegels also decrease your chances of pelvic organ prolapse (POP) and constipation. Use a guide to learn how to do pelvic floor exercises or see a pelvic floor therapist.
2. Bladder Control Products
Bladder pads, adult briefs, or adult protective underwear can help you regain confidence while experiencing UI symptoms. These products control urine leaks and odor with their highly-absorbent material, keeping you cool and dry throughout the day.
Aeroflow Urology may be able to provide you with these supplies for free through insurance if you qualify! See if you’re eligible to get them today with our Eligibility Form.


3. Bladder Training
Bladder training retrains your bladder muscles to hold urine for more extended periods. It consists of going to the bathroom at scheduled times and holding your pee when you feel the urge to go.
4. Nutrition & Exercise
Avoid bladder irritants, such as smoking, alcohol, caffeine, spicy foods, and citrus fruits to decrease UI symptoms. Exercising regularly strengthens pelvic floor muscles and keeps things running smoothly.
5. Medication
Certain medications or Botox injections calm your bladder, decreasing OAB symptoms. You can also get collagen injections that will thicken your bladder to improve symptoms of UI.
6. Hydration
Drinking enough water (about 11 cups a day for women) flushes out toxins and bacteria, decreasing the risk of developing UTIs. And, contrary to what you may think, staying hydrated decreases incontinence symptoms. This is because dehydration causes your urine to become more concentrated, which irritates the bladder.


7. Topical Creams
Vaginal creams with estrogen can be applied to your vagina and aid in reversing UI symptoms caused by early or temporary menopause.
8. Support Groups
Incontinence significantly impacts women’s mental health, so virtual or in-person support groups may help you during breast cancer treatment, recovery, or if you’re experiencing UI symptoms.
Get Free Bladder Control Products
At Aeroflow Urology, we know that managing incontinence along with pre-existing medical conditions can be stressful. That’s why we offer bladder control products for women through insurance if they qualify!
We send free product samples, connect you with an expert Continence Care Specialist to answer any questions, and send your supplies for free no matter where you live.
You’ll get your products in discreet boxes every month, so you won’t need to go to the store to buy them.
To see if you qualify, fill out our 2-step Eligibility Form. It takes under 5 minutes. Just have your insurance card at hand.
High Prevalence of Urinary Incontinence With Breast Cancer Suggests Potential Overlap of Risk Factors. (2020, June 29). Oncology Nurse Advisor. https://www.oncologynurseadvisor.com/home/cancer-types/breast-cancer/risk-factors-for-breast-cancer-may-overlap-with-those-for-urinary-incontinence/#:~:text=Urinary%20incontinence%20was%20highly%20prevalent
Urinary problems in women | Coping with cancer | Cancer Research UK. (n.d.). Www.cancerresearchuk.org. Retrieved July 26, 2022, from https://www.cancerresearchuk.org/about-cancer/coping/physically/sex-hormone-symptoms/women-coping-with-hormone-symptoms/urinary-problems
Stahlschmidt, R., Ferracini, A. C., Medeiros, L. M. de, Souza, C. M. de, Juliato, C. R. T., & Mazzola, P. G. (2020). Urinary Incontinence and Overactive Bladder Symptoms in Women with Breast Cancer Being Treated with Oral Hormone Therapy. Revista Brasileira de Ginecologia E Obstetrícia / RBGO Gynecology and Obstetrics, 42(11), 726–730. https://doi.org/10.1055/s-0040-1718440
Carter, D. (n.d.). 7 things to know about menopause and breast cancer. MD Anderson Cancer Center. Retrieved July 26, 2022, from https://www.mdanderson.org/cancerwise/7-things-to-know-about-menopause-and-breast-cancer.h00-159306990.html#:~:text=Chemotherapy%20can%20cause%20temporary%20menopause&text=Women%20receiving%20chemotherapy%20%E2%80%93%20regardless%20of
Urinary Incontinence an Often Unrecognized Cancer Complication. (1998). Www.cancernetwork.com, 7(6). https://www.cancernetwork.com/view/urinary-incontinence-often-unrecognized-cancer-complication
Incontinence, pelvic pain, constipation, and sexual dysfunction associated with breast cancer. (n.d.). Lovelace Cancer Center. Retrieved July 26, 2022, from https://lovelacecancercenter.com/blog/incontinence-pelvic-pain-constipation-and-sexual-dysfunction-associated-breast-cancer
Information provided on the Aeroflow Urology website is not intended as a substitute for medical advice or care from a healthcare professional. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.








