This blog was updated on 10/06/2023.
Post-traumatic stress disorder (PTSD) is a complicated and intense mental health battle many adults face in silence. Its well-known symptoms, like nightmares, anxiety, depression, and flashbacks, make this condition an incredible challenge for those experiencing it. But, another symptom can make recovery even more difficult— one that can profoundly affect individuals' mental and physical health.
Urinary incontinence, or the loss of bladder control, is an often overlooked symptom in many adults with PTSD. This bladder condition can make the struggles of PTSD heavier for some, especially since urinary incontinence is not discussed very openly in our society.
In this article, we'll explore the reasons you may experience incontinence with PTSD. We'll tell you how to manage your symptoms and seek help so you have the tools to improve your mental and bladder health.
What Is PTSD?
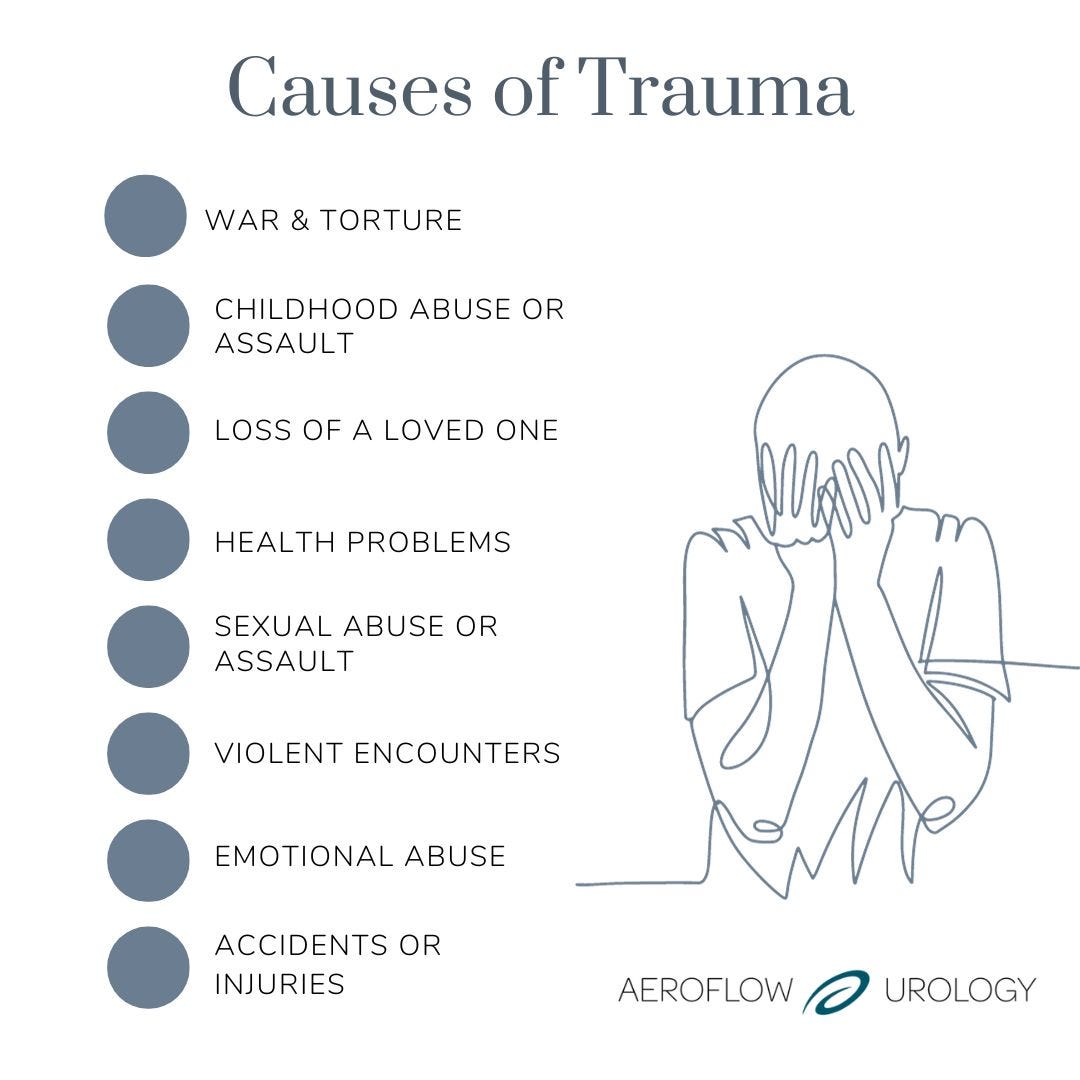
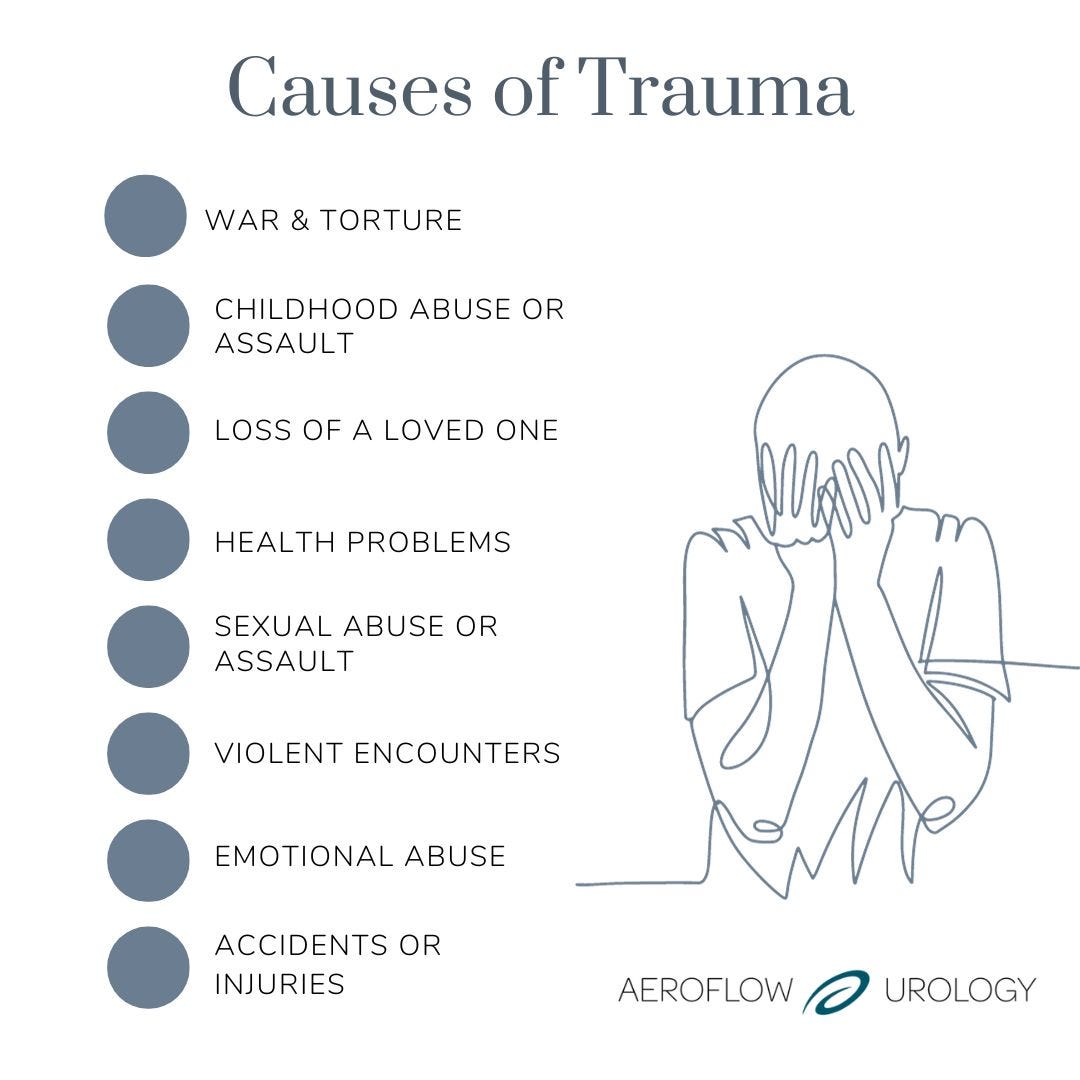
Trauma is an emotional response to a life-changing event that can cause someone to experience shock, denial, flashbacks, dysregulated emotions, strained relationships, and a myriad of challenging physical symptoms.
It's reported that 70% of people in 24 countries have experienced a traumatic event, and around 30% have experienced as many as 4 traumatic events in their lifetimes.
Causes of trauma can include (but are not limited to):
Check Your Eligibility
2 Easy Steps
From catheters to pediatric and adult incontinence supplies, discover the continence care essentials covered by your insurance.
- War and torture.
- Childhood abuse or assault.
- Loss of a loved one.
- Serious health problems.
- Sexual abuse or assault.
- Violent encounters.
- Emotional abuse.
- Accidents or injuries.
After living through trauma, people may sometimes experience post-traumatic stress disorder (PTSD). PTSD is a mental health condition triggered by a traumatic event that an individual was involved in or witnessed. Often, a person will have difficulty recovering after the terrifying experience and feel stressed or frightened, even when they're not in immediate danger.
About 1 in 3 people who live through trauma develop PTSD, but it isn't currently known why only certain people develop the condition while others do not. The mean age of individuals experiencing PTSD is 23, with young people and those in middle adulthood more likely to experience it. PTSD is widely known among veterans who have been on active duty. One study showed that around 12% of U.S. veterans were diagnosed with the condition. This number includes men and women veterans. A women's health study also found that among female veterans, 19% reported having urge or mixed incontinence.
It's also common for people to experience PTSD after sexual assault or abuse. One study showed that 75% of sexual assault survivors were diagnosed with PTSD a month after the assaults. Another study showed that more than 20% of women who reported a history of PTSD experienced urinary tract dysfunction.
The Journal of Urology also found that among women diagnosed with PTSD:
- 45% reported incontinence.
- 23% said stress urinary incontinence.
- 23% reported urge incontinence.
- 35% reported nocturia (bedwetting).
The severity and type of PTSD may vary due to various contributing factors. A person may have:
- Short-term (acute) PTSD: Lasting for around 6 months.
- Ongoing (chronic) PTSD: Lasting for more than a year.
It isn't totally clear to healthcare professionals why PTSD occurs, but it's suggested that it happens due to:
- Your body attempting to keep you alive. Some research suggests that PTSD develops to keep you alive if the traumatic or life-threatening situation were to occur again. With the flight-or-fight response activated in your body, you can react more quickly and are more likely to survive.
- Changes in your hippocampus. Your hippocampus is a part of the brain responsible for memory and emotion. It's been found that in people with PTSD, their hippocampus is smaller. This is believed to be due to anxiety or fear.
The risk factors for developing PTSD include being predisposed to anxiety and depression.
Symptoms of PTSD
- Re-experiencing symptoms through flashbacks or nightmares.
- Avoiding event reminders (such as riding in a car after a car accident).
- Experiencing angry outbursts or insomnia.
- Feeling on edge and guilty.
- Having issues recalling events surrounding the incident.
- Being in a perpetual state of flight-or-fight.
Nocturnal enuresis, nighttime bedwetting, and urinary incontinence are also symptoms, especially in children, even if they've already been potty trained.
Can Urinary Incontinence Be Caused by PTSD?
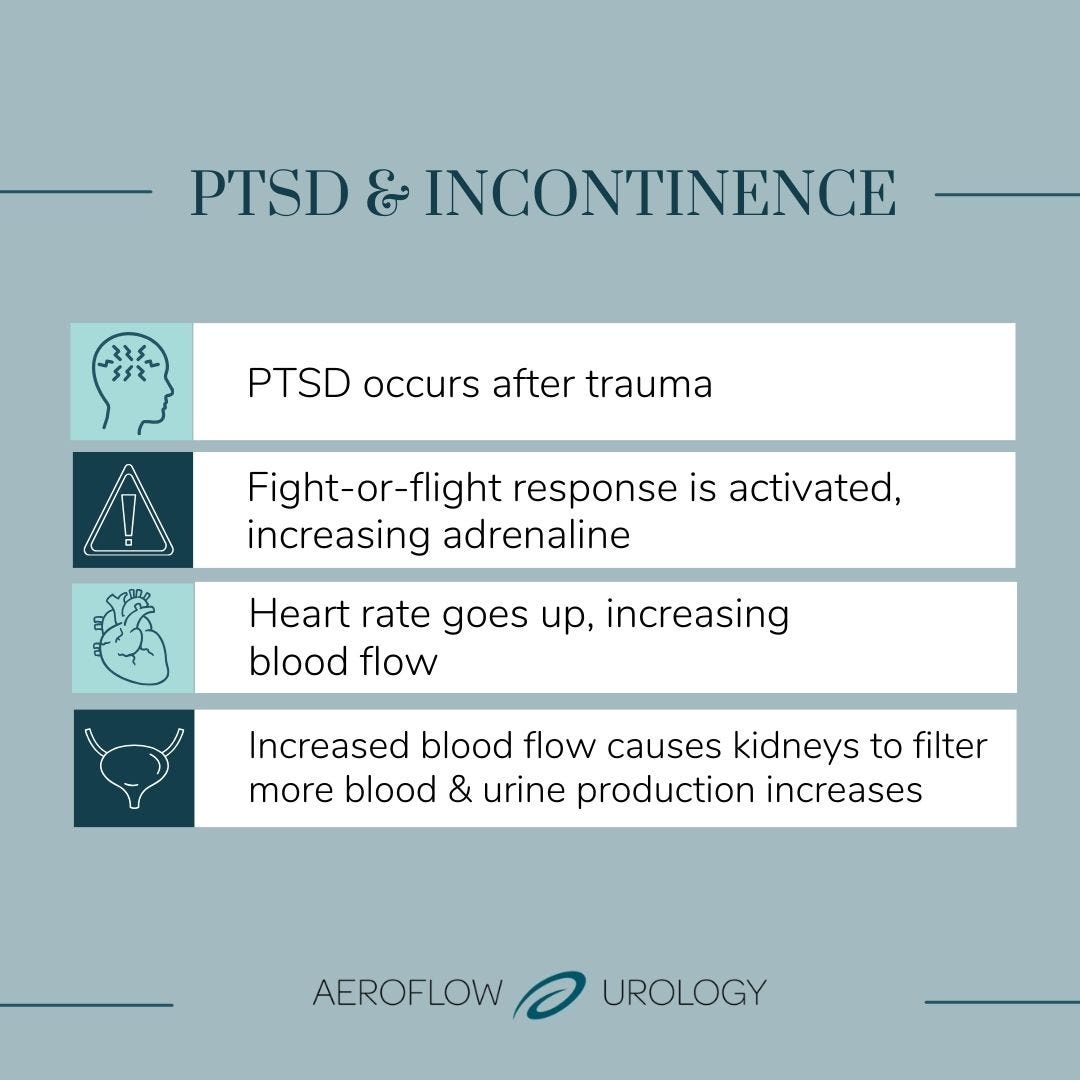
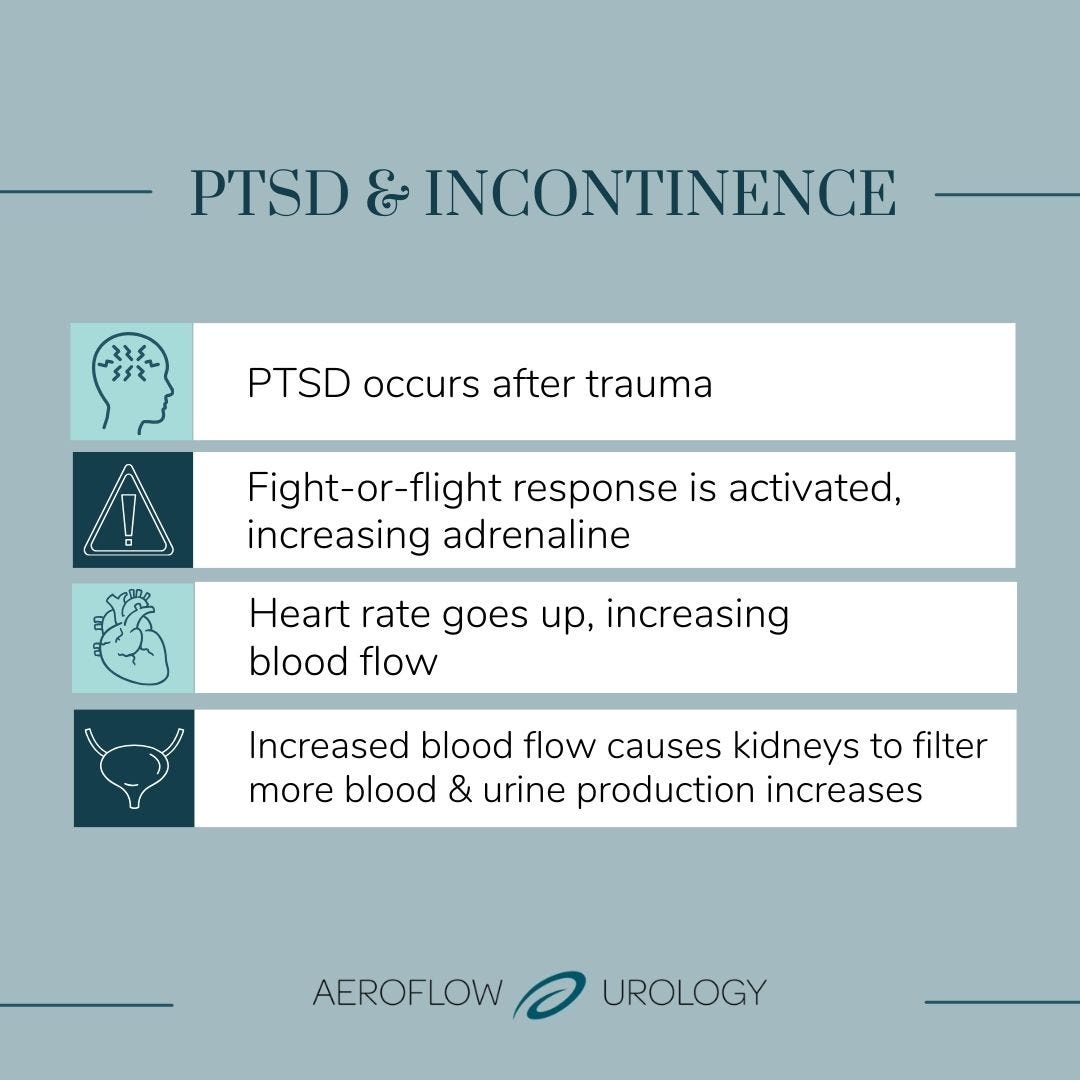
Reliving trauma and the anxiety it puts on your body can activate the sympathetic nervous system, known as the fight-or-flight response. During fight-or-flight, your body creates more of the stress hormone, adrenaline, and your body's nerves are triggered, making you less prone to feeling pain and quicker to react to threatening stimuli.
When this adrenaline fills your body, your heart rate increases, causing more blood flow. Due to more blood flowing through your body, the kidneys filter more blood, increasing urine production, which causes the bladder to fill faster.
Therefore, the bladder muscles tense up and contract, increasing pressure on the bladder, which signals urine release. This causes bladder dysfunction and urinary incontinence.
Urinary incontinence is the loss of bladder control, and the condition affects many people but is not normal. While there are different types of incontinence, such as stress urinary incontinence and overactive bladder, PTSD is usually mostly related to urge incontinence.
Urge incontinence occurs when you feel the sudden, unexpected urge to urinate. It may be impossible to reach the bathroom when this urge comes about, leading to urine leakage. Urge incontinence may also lead to urinary frequency or bedwetting.
How Do You Treat PTSD & Urinary Incontinence?
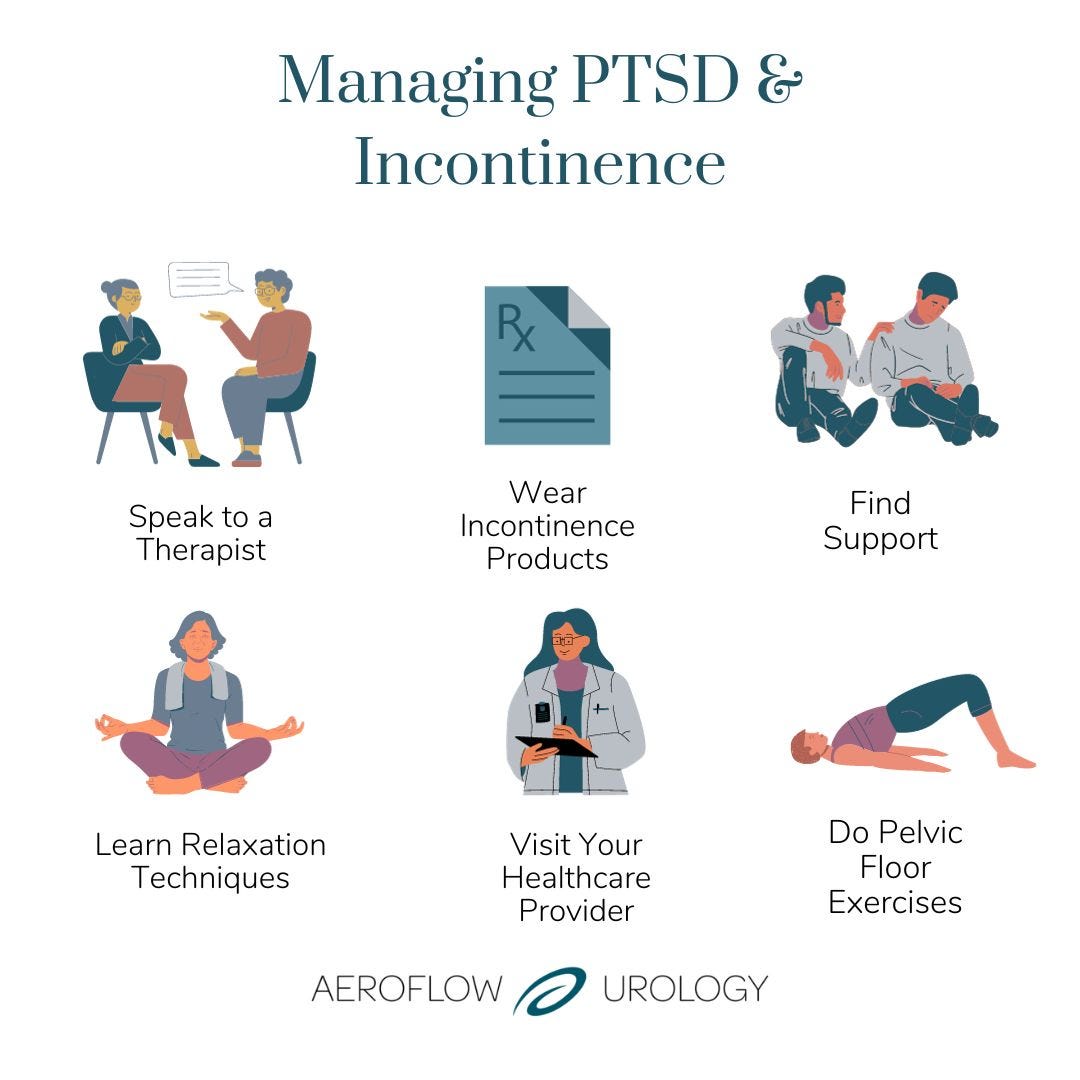
Episodes of urinary incontinence are common in individuals with PTSD, so having the right tools to manage them is essential. There are a variety of PTSD treatments available, but you also want to ensure that your incontinence symptoms are also treated. It's important to remember that incontinence can be a source of anxiety and embarrassment, and this anxiety can exacerbate symptoms further. The following tips can help you manage PTSD and symptoms of urinary incontinence.
Speak With a Therapist
It can be an excellent option to meet with a therapist to evaluate your symptoms. Talk therapy can help identify triggers that may be causing the incontinence to occur, along with cognitive behavioral therapy treatments to improve PTSD symptoms.
Wear Incontinence Products
If you are managing incontinence alongside PTSD after living through trauma, incontinence products may be able to alleviate some of the anxiety, shame, and stress away from your everyday life.
Products like adult pull-ons and bladder control pads may be beneficial in the case of urge incontinence by keeping you dry when leakage occurs. These products are highly discreet and are made to look and feel like real underwear. You may also be eligible to get free incontinence products through your insurance and Aeroflow Urology. See if you qualify for free incontinence supplies in under 5 minutes.
Find Support
It may make managing symptoms easier if you can be open with people about your PTSD and urinary incontinence symptoms. Find someone you trust, such as a therapist, a close friend, a loved one, or a support group, and talk about your experiences. The Department of Veterans Affairs is another support group that may be helpful to veterans managing these conditions.
Learn Relaxation Techniques
Relaxation techniques, such as deep breathing, yoga, and meditation, are incredibly beneficial if you struggle with an incontinence episode or PTSD. Yoga can also help with regaining control of your pelvic floor.
It can be difficult to calm yourself during stressful moments. However, it's recommended that you practice relaxation techniques before an episode occurs to help deactivate the sympathetic nervous system, restoring the body to a rest or digest state. This can also be an excellent technique for calming PTSD episodes, especially in children.


Visit Your Healthcare Provider
While your PTSD may cause your incontinence, incontinence can also be a symptom of a bladder condition or a urinary tract infection (UTI). A visit to your healthcare provider can be beneficial in treating or managing your symptoms. Your provider may also be able to help you find a therapist or other local or online support groups.
Do Pelvic Floor Exercises
If you're managing incontinence, pelvic floor therapy or pelvic floor exercises will help you gain strength in your pelvic floor muscles, which can improve incontinence symptoms. You can do these exercises in the comfort of your own home or with a group or therapist. Exercise can also help decrease the symptoms of PTSD by lessening anxiety and stress and increasing the hormones that make you happy.
How to Get Discreet Incontinence Products to Manage PTSD & Urinary Incontinence
Whether you or your loved one needs bladder control pads, underpads (chux), or protective underwear, Aeroflow Urology can assist with receiving incontinence products through your insurance. This can help relieve some of the incontinence's financial stress, make accidents easier to manage, and bring back a better quality of life.
Returning to your routine can be more achievable once you find the right incontinence products for your needs. This can also alleviate stress and give the individual confidence that they are protected and covered if an accident occurs.
Once approved, one of our Continence Care Specialists will contact you to answer questions, help you complete the necessary paperwork, and send free product samples. After you've chosen your supplies, they'll be sent directly to your home in discreet packaging every month.
References
Boyd, B. A. J., Gibson, C. J., Van Den Eeden, S. K., McCaw, B., Subak, L. L., Thom, D., & Huang, A. J. (2020). Interpersonal Trauma as a Marker of Risk for Urinary Tract Dysfunction in Midlife and Older Women. Obstetrics and Gynecology, 135(1), 106–112. https://doi.org/10.1097/AOG.0000000000003586
NHS. (2021, February 17). Post-traumatic Stress Disorder. Nhs.uk. https://www.nhs.uk/mental-health/conditions/post-traumatic-stress-disorder-ptsd/overview/
Trauma and Its Aftermath | SPH. (n.d.). Www.bu.edu. Retrieved May 4, 2022, from https://www.bu.edu/sph/news/articles/2018/trauma-and-its-aftermath/#:~:text=Traumatic%20events%20are%20a%20near
How Exercise Can Help Your PTSD Mentally and Physically. (n.d.). Verywell Mind. https://www.verywellmind.com/exercise-for-ptsd-2797465
Nodell, B. (2021, July 20). 75% of sexual assault survivors have PTSD one month later. Newsroom.uw.edu. https://newsroom.uw.edu/news/75-sexual-assault-survivors-have-ptsd-one-month-later
Hill and Ponton. (n.d.). PTSD and Veterans: Breaking Down the Statistics. Hill & Ponton, P.A. https://www.hillandponton.com/veterans-statistics/ptsd/
Lee, L. (n.d.). PTSD and Aging. https://www.ptsd.va.gov/publications/rq_docs/V30N4.pdf
PTSD Linked to Urinary Incontinence in Female Veterans. (2012, June 1). MPR. https://www.empr.com/home/news/drug-news/ptsd-linked-to-urinary-incontinence-in-female-veterans/
Boyd*, B., Gibson, C., Eeden, S. V. den, McCaw, B., Subak, L., Thom, D., & Huang, A. (2019). PD31-07 INTERPERSONAL TRAUMA: AN UNDER-RECOGNIZED RISK FACTOR FOR SYMPTOMATIC URINARY TRACT DYSFUNCTION IN MIDLIFE AND OLDER WOMEN. Journal of Urology, 201(Supplement 4). https://doi.org/10.1097/01.ju.0000556184.47145.af
Disclaimer
Information provided on the Aeroflow Urology blog is not intended as a substitute to medical advice or care. Aeroflow recommends consulting your healthcare provider if you are experiencing medical issues relating to incontinence.